WHO defines empowerment as “a process through which people gain greater control over decisions and actions affecting their health” (WHO 1998). This shift is due in large part to the use of technology that facilitates increased patient access to information and ability to communicate via the Internet, peer-to-peer sharing, consumer health devices, and mobile apps.
Increasingly, healthcare providers have opportunity to remotely collect and utilise patients’ personal health data, such as data from their home-use medical devices and wearables, within healthcare services. Such personal health data can provide deeper insight into patients’ own health metrics, lifestyle decisions and behavioural trends, thus expanding patient data previously collected on clinical sites. During the coronavirus pandemic, the ability to capture such data in near real time from individuals remotely is vital to managing the pressure on healthcare services.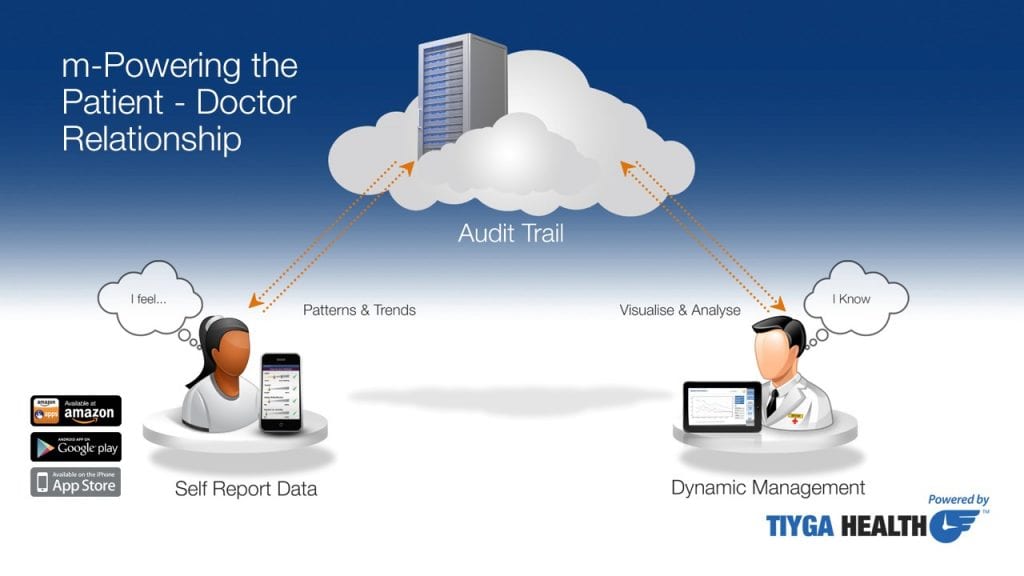
A high proportion of consultation time can be spent on taking a history. Yet, this process depends on several factors; how articulate the patient is, how well they recall their experiences, and how long it has been since the past consultation etc. As problem-solvers, clinicians can only do their best with information the patient gives them. Better input enhances health outcomes.
The voice of the patient – without white-coat syndrome
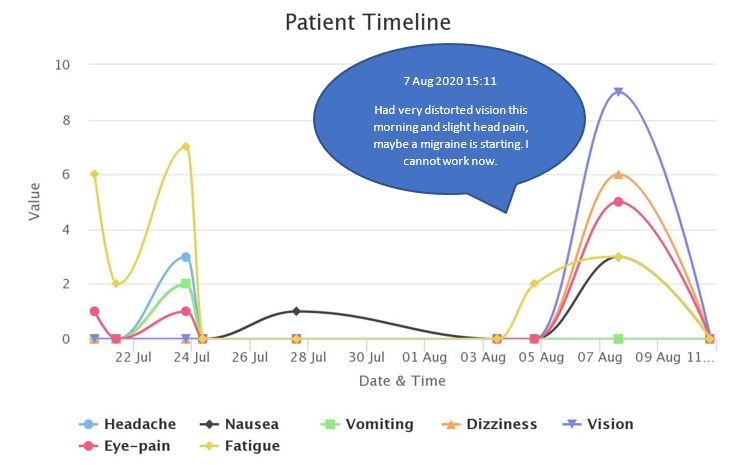
Often patients bring their own detailed “diary” observations, but they are frustrated when clinicians do not have time to look at this personal evidence. TIYGA software provides a structure to engage patients more efficiently and more effectively and also empowers the patients to contribute their experience and knowledge. It also gives opportunity for healthcare professionals to review those data in a systematic way and examine individual longitudinal trends. There are currently no sensors to measure every symptom objectively; clinicians rely on self-report. Patients have the burden of remembering the sequence of events and then to recall this accurately for each and every clinician they meet under time-schedule pressure. Being able to “offload” these observations privately, securely, and conveniently in their own terms is a relief. A problem shared is a problem halved.
TIYGA captures, measures, analyses and charts self-report data that reflects the authentic voice of the individual patient. Talking takes time but that information can be captured asynchronously and displayed privately and conveniently. The aim is to support timely and meaningful interventions according to clinical need, without requiring high tech kit or extensive health literacy or exposure to the risk of leaving a secure setting. The healthcare professional can view the patient-generated data immediately they are recorded by the patient.
TIYGA software provides a patient-friendly way of recording lived experience within a format that allows professionals to compare cohorts of patients and make safer decisions. TIYGA was designed around the individual (disease-agnostic, holistic) and the only requirement is for the patient to have a smartphone (with a good signal) and a basic level of technology and health literacy. TIYGA makes it easy to record relevant data within a convenient format and to view charts that help them to see the relationship between the choices they make (e.g. taking medication, exposure to triggers, daily activities) and the symptoms that impact on the quality of their life. TIYGA complements other forms of patient-provider communication, it complements video, email, web, and face to face approaches.
Patients become empowered and more vigilant of their health status by becoming actively engaged; but this remote connection to the professionals who understand the right treatment options, gives more confidence and reduces anxieties enabling the patient to respond to the challenges ahead. This is equally true for people with pre-existing or newly emerging conditions, for women who become pregnant or those who think they may have some form of coronavirus or rehabilitating from having had a severe form of COVID-19. Consumer medical devices give part of the story, the rest is verbal self-report.
Individual behaviour plays a major role in determining the spread of the virus and we do not yet understand what makes some people get a more severe form of COVID-19. Indeed, researchers have identified six clusters of symptoms with very different outcomes. The ability to triage and direct people to the right resources in a timely manner is critical.
People’s time is an asset – make best use of it – delays cost lives
During the COVID-19 crisis, waiting times for specialist treatment rose to an average of 15.3 weeks in the UK in May 2020. Only 220,000 elective general and acute admissions occurred in May – a dramatic change from the monthly norm of approximately 700,000.
Statistics from the Royal College of General Practitioners found, in the four weeks leading up to 12 April 2020, that 71% of routine consultations in general practice were delivered remotely. According to NHS Digital, in 2019, just 13% of NHS GP appointments in England were held over the phone and less than 1% took place via video/online. One in twenty (5%) GP appointments were recorded as ‘did not attend’ in 2019. COVID-19 has accelerated the uptake of video consultations but there remains an opportunity for more history-taking to be carried out asynchronously with patients reporting the progress of their symptoms on their smartphones and clinicians having reports at their fingertips when they need them.
TIYGA is an acronym for Time Is Your Great Asset – it is designed around the individual to bring patient knowledge to healthcare professionals in a timely way, in near real time, asynchronously. The aim is to support problem-solving. Every healthcare professional has many patients to care for and they cannot watch over every patient in real time. But they do have the knowledge to decide when someone is stable, improving or deteriorating via triage according to clinical need.
Time is critical for anyone living with cancer, heart disease, diabetes, or any long-term condition – getting the right treatment at the right time and place, by the right person is essential. Delays cost lives, timely intervention relies on timely and trusted information. One size does not fit all. Health services are aiming to deliver person-centred care and personalised medicine, getting it right first time. The data reported by individual patients is increasingly seen as vital to achieving this.
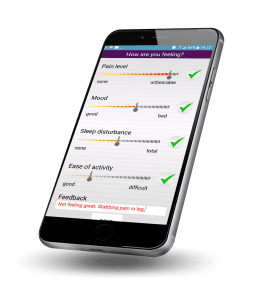
TIYGA apps are designed to be simple, quick and easy for patients to report on what they are experiencing in as short a time as possible and within a template controlled by the healthcare professional (fine-tuned to be relevant to the current problem). The TIYGA dashboard allows each healthcare professional to create app accounts that are tailored to their patient and to display the reports they need to triage patients and to have conversations that are in a language that more patients understand.
TIYGA apps allow people to keep a diary of observations and lived experience. For example, the events leading to flare-ups which could result in visits to urgent care, to avoid recall error and keep a note of their own triggers and self-management solutions. The apps can be focused on symptoms or activities and allow free text input to let the patient report specific observations in their own words. This often provides rich insights that might not emerge through established questionnaires. It is often noted that the comments patients make on the way out of consultations turn out to be particularly relevant, TIYGA provides a way to report these details.
This is particularly true for those with a high motivation to help themselves, to avoid over-medicalisation and reliance on medication. TIYGA apps offer convenient communication asynchronously which does not disadvantage those who take longer to articulate how they are feeling or who do not like talking about embarrassing matters face to face. In a similar way, those who are disfigured or have a speech impairment may prefer the TIYGA approach. TIYGA gives a voice to those who are hard or hearing or whose disability makes it difficult to attend consultations in person and those who are very anxious and really need to tell somebody about their worries. TIYGA apps let patients enter data when convenient to them; and by not being face to face, any fear of bias due to ethnicity or gender is minimised. When people delay seeing a doctor, it may minimise options of treatments the clinician could offer. While resources are under pressure, it is more important than ever to reduce the number of patients who do not attend consultations.
TIYGA is not replacing emergency or any healthcare service. It augments existing services with a light touch way to capture longitudinal data with least recall error. It can help most where symptoms vary over time. TIYGA data should be used in combination with other data that the healthcare provider has, including clinically validated objective measures. TIYGA records the data in a form that can be analysed and triaged. Some people feel guilty about taking valuable clinical time. Even without COVID-19 there were many reasons why people did not engage with healthcare providers.
All patients are not the same, and they don’t all communicate the same way, some are more proactive, and others are more reactive. COVID-19 has increased the importance of individuals being more engaged in their own healthcare. When patients see the positive impact of their behaviour on their clinical health measurements, they can believe they are more in control rather than just a victim of the disease. TIYGA increases engagement of patients and empowers the patient-doctor relationship – without the need to be in the same place or online at the same time.
In the shadow of COVID-19 we need to be agile and learn in real time
Before this crisis, around 85% of the burden of disease in the UK was from long term conditions such as cancer, heart disease and depression. Women’s access to services for their condition fell by 4% more than for men and the drop off in services was slightly more pronounced for those over 55.
There was a 30% fall in emergency admissions in May 2020 compared with May 2019. Access to health services in the UK for people with pre-existing conditions was 20% lower and some of the largest falls in use of health services were for cancer and mental health, falling 25% and 22% respectively. Surveys showed that 47% of people would feel uncomfortable using their local hospital in the short term if the need arose and 76% were concerned about being exposed to COVID-19.
The pandemic is likely to result in a series of discontinuous changes that will fundamentally reshape healthcare including the need to be able to flex up and down care capacity and shift care across modalities, including virtual health platforms. TIYGA’s cloud-based ecosystem can be used to share data with healthcare professionals at multiple locations and so provide flexibility in response in a situation where responsiveness is essential.
Clinically sick patients will have even less energy or inclination to navigate complex forms or tolerate time consuming questions. Many apps are designed to be so comprehensive that they can become over-complex for those least confident with technology or who are feeling most unwell. Against a background of a highly infectious and sometimes deadly virus, patients want a convenient and immediately obvious way to report on how bad their symptoms are at a specific the time; TIYGA technology was designed to be very easy to use.
“An app such as this, that will enable someone suffering the daily, seemingly endless, challenges of a chronic illness to understand that illness a bit better can only be a good thing. The fact that this app is designed specifically and intentionally to allow both the patient and their doctor to collaboratively develop an understanding of the illness has far reaching potential that could well begin to bridge a decades long gap to renewed trust and hope.”
Paddy, Host and Producer, It’s Not All About ME Podcast and Hope 4 M.E. and Fibromyalgia Northern Ireland member.
Many people do not want to be continuously monitored and will not use, or cannot afford, wearable or home-based ambient trackers, but they have increased anxiety because of COVID-19 and need to feel supported rather than alone. With a backlog of demand for services that were stopped or at reduced capacity for three to six months, the need for digital triage and light touch solutions for large numbers of people is becoming more urgent. The TIYGA dashboard signals which patients have reported high scores in the past 24hrs making it easier for healthcare professionals to prioritise according to need and identify those that need attention.
Automation can increase the efficiency and effectiveness of health services to deliver person-centred care by using the personally meaningful and actionable data reported by patients. This must happen within a structure that is managed by healthcare professionals.
COVID-19 has accelerated collaboration and learning by researchers, healthcare professionals and administrative bodies around the world. Now it is time to bring the knowledge of patients into healthcare services in near real time, to help clinical teams to achieve the best possible health outcomes.