Dr Zemphira Alavidze, a medical microbiologist at Phage Therapy Center, explains the benefits and challenges associated with phage therapy.
Phage Therapy Center was founded in 2003 by a leading group of Georgian microbiologists and polymer scientists. Their goal was to establish a clinic that catered to foreign patients primarily to treat non-healing / chronic wounds. The clinic was acquired by Phage International, who funded a treatment facility in Tbilisi and expanded the scope of treatment to the most common chronic and drug-resistant infections.
Phage Therapy Center has treated around two thousand foreign patients, half of which have travelled to Georgia for treatment and half – where appropriate or there are no travel options – are treated remotely. The clinic has handled over 50,000 communications with patients seeking treatment for drug-resistant / chronic infections. Health Europa spoke to medical microbiologist at Phage Therapy Center, Dr Zemphira Alavidze, to find out more about phage therapy, its associated benefits and challenges.
How would you describe phage therapy?
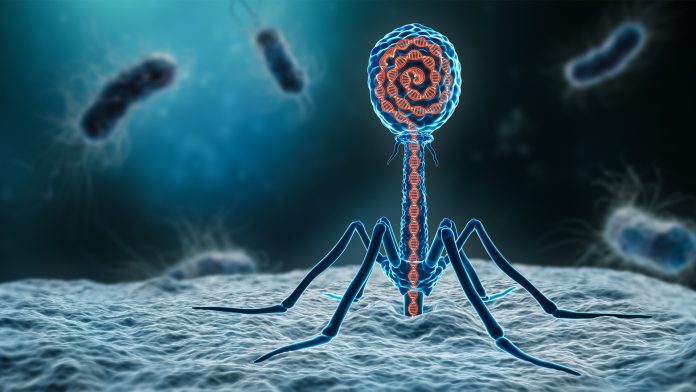
Phage therapy is the therapeutic use of select lytic bacteriophages to biocontrol specific strains of bacteria. It is a mechanism for eliminating the specific bacteria that cause an infection. Bacteriophages or ‘phages’ are a particular class of viruses that only infect bacteria. Lytic bacteriophages insert themselves and replicate inside of their bacterial host. They then release a lytic enzyme that causes the cell wall to rupture, thereby killing the bacterium and releasing multiple progeny phages. The term ‘biological control’ or ‘biocontrol’ means controlling one type of organism with another predator-type organism. It relies on natural mechanisms but typically also involves an active human management role.
Because we are dealing with biologics as opposed to small molecule drugs (like antibiotics, which destroy the patient’s microbiome, and which tend to make the condition worse in the long run), phage therapy is a means of targeting specific strains of bacteria in the infection. The phage preparation itself must be capable of dealing with situations whereby the bacterial pathogen will try to mutate in order to survive the attack on it by the phages. Usually, a well-designed phage cocktail will continue to fight the infection, but it is necessary to continue to monitor this during treatment to make sure the infection has not morphed resistance to the phages.
Unfortunately, in chronic patients, unless the patient makes lifestyle changes to improve their immunity, they may again become infected with an opportunistic pathogen. The same is true with antibiotics, but the difference is antibiotics tend to kill large swaths of the microbiome and phages only kill or ‘control’ the specific strain targeted by the therapy.
It is well defined in literature that antibiotics fail consistently when there is an attempt to deal with chronic/biofilm-based infections. Bacteriophages, on the other hand, can disrupt biofilms and ultimately clear an infection. Once the biofilm begins to collapse, the infection can begin to respond to antibiotics. It is our experience that antibiotics and phages are highly compatible and, when used properly, can together provide the patient with an excellent result.
What types of conditions can you treat at the centre?
Generally, our clinic treats the following pathogens:
• Escherichia coli (E.coli)
• Enterococcus (multiple species)
• Klebsiella (multiple species)
• Morganella (multiple species)
• Salmonella (multiple species)
• Staphylococcus (multiple species)
• Streptococcus (multiple species)
… and several others that cause the following medical conditions, both acute and chronic (biofilm-caused) including:
• Acne
• Bed Sores
• Bronchitis
• Burns (infected)
• Chronic Fatigue Syndrome
• Chronic / Non-healing / Infected Wounds
• Colitis
• Cystic Fibrosis
• Diabetic Foot
• Laryngitis
• Lung Infections
• Rosacea
• Tropic Ulcers
• Urinary Tract Infections (UTI) and Cystitis
• Vaginitis
• … and several others
What are the primary challenges currently facing the management and treatment of bacterial infections?
As there is more than a hundred-year history of use of bacteriophages in Georgia, the technical issues are for the most part understood and generally resolved.
Antibiotic resistance occurs when bacteria change in response to medicines and develop the ability to defeat drugs. While antibiotic resistance occurs naturally, the overuse and misuse of antibiotics has accelerated the process. They lead to longer hospital stays, higher medical costs and more otherwise preventable deaths. Therefore, antibiotic resistance has been identified by the WHO as one of the biggest threats to global health.
Most pharmaceutical companies are no longer working on new antibiotics. Half of all antibiotics used today were discovered during the 1950s. Since that time, discovery and development of antibiotics has become more complex, time-consuming, and expensive. New antibiotics that are approved typically have short treatment durations and restrictions on their use to slow the emergence and spread of resistance. This limits their profitability. Even when new antibiotics are made available, they rarely target priority drug-resistant bacteria and are only registered for use in a small number of countries.
Regarding phage therapy, of course, there are challenges, and one of them is the preparation of injectable phages, which requires the introduction of high-tech processes, around which countries with extensive experience (such as Georgia and Poland) and countries with strong technologies, in general, should be united.
From a logistical perspective (management), which affects the ability of patients in both North America and Europe: for many years, Phage Therapy Center was able to provide bacteriophages to US and European patients under the compassionate use ‘policies’ provided by FDA and equivalent regulatory agencies. This policy, for some unknown reason, was recently revoked without notice in the United States.
So, our primary challenge has been regulatory, which is surprising because lytic bacteriophages are categorised by FDA as ‘Generally Recognised as Safe.1 There seem to be two approaches to phage therapy that are evolving in our medical establishments2, each with its own set of challenges: broad spectrum phage cocktails (the Soviet methodology) and custom phage preparations, where a custom product is designed for each patient.
The Georgians utilise both methods. In the past, typically, five to 10 patients per month had custom phage products developed for them in cases where their infections were resistant to the commercially available phage cocktails. However, the current commercial products produced by the two Georgian manufacturers work in most cases.
Outside of Georgia – and this is supported by the fact that, to date, no broad spectrums brought to clinical trials in the US and Europe have passed phase 2 clinical studies – developers have not yet figured out how to design broad spectrum cocktails. There is such variation in the sensitivity of strains encountered in clinical practice. Keeping up with the ongoing evolution of resistance is a product maintenance issue that totally breaks down in the traditional drug approval model.
Can you tell me about any recent novel technologies, methodologies or protocols that have improved the treatment of chronic infections?
Bearing in mind that most of our patients are chronic and typically immune compromised – for various reasons including age and overuse of antibiotics – the presence of biofilm in various infected locations in the body that render antibiotics ineffective complicates the patient condition.
While we do not consider phage therapy to be a panacea, phage therapy is applicable for bacterial infections such as sinusitis, otitis, urinary tract, prostatitis, non-healing wounds, including diabetic ulcer, vaginitis, intestinal infections, bronchitis, acne, and others. But it is not just the phages that ultimately improve the condition. It is a combination of protocols not just to clear what may be a pathogen or group of pathogens that can morph during treatment – there needs to be a holistic approach that may include treatment of the immunology as well as certain lifestyle modifications.
References
- Bacteriophages are ubiquitous in the environment, there are more types of phages in our ecosystem than all other species combined. They cover everything and coexist in perfect harmony with all life forms EXCEPT bacteria. Since we are constantly encountering phages in everything we consume and touch, of course no harm can come to higher life forms from these organisms
- Actually there is a third one and that is GMO phages









