Prostate Cancer UK Senior Specialist Nurse Emma Craske speaks with HEQ about the diagnosis and treatment of prostate cancer.
Founded in 1996 as the Prostate Cancer Charity, before merging with Prostate Action UK in 2012, Prostate Cancer UK was the UK’s first national organisation focusing on prostate cancer. In the last 20 years, the charity has invested more then £66m in research; and it continues to provide support for men with the disease and their families, as well as raising awareness of prostate cancer and campaigning to improve patient care. Emma Craske, Senior Specialist Nurse at Prostate Cancer UK, speaks with HEQ about prostate cancer care, treatment and innovation in the sector.
How common is prostate cancer in the UK? What treatments are indicated?
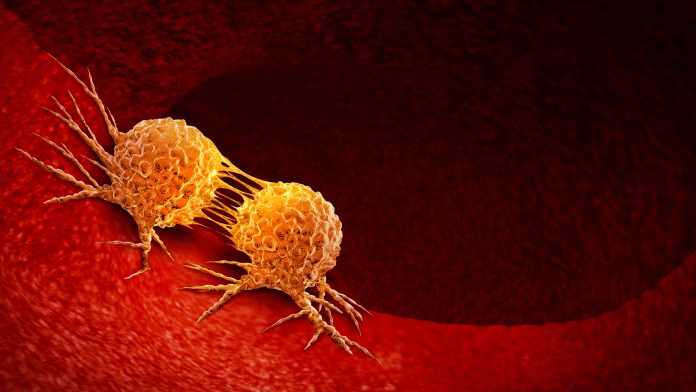
More than 11,500 men die from prostate cancer in the UK each year: it is the most common cancer in men; and it is the most commonly diagnosed of all cancers in the UK. One in eight men across the general population of the UK will be diagnosed with prostate cancer; that figure rises to one in four for black men. There is research being conducted to try and determine why prostate cancer is more prevalent in black men, but we do not yet have a complete answer – prostate cancer is quite complex, but there is a growing body of work examining the various mutations and the science is moving ahead.
Not every man who is diagnosed with prostate cancer will need treatment. Some slow-growing, low-risk prostate cancers do not need to be treated immediately, so they are observed; then, if the nature of the cancer changes, those men can be offered potentially curative treatments. This process is called active surveillance. In patients who do need treatment, the type of therapy offered will depend on where the cancer is: some men will need to have surgery to remove the prostate; some men will have hormone therapy and radiotherapy. There are newer treatments available called focal therapies: these are for men whose cancer is contained in the prostate; rather than treating the whole prostate, they treat targeted spots of cancer. High-intensity frequency ultrasound (HIFU) kills cancer cells by directing heat at them, while cryotherapy freezes spots of cancer within the prostate. In cases of metastatic prostate cancer, where the cancer has spread further afield, patients may need systemic treatments which can treat the cancer wherever it is in the body – this may entail longer-term hormone therapy and possibly some chemotherapy.
These days, there are a whole sequence of potential treatments which could be considered for men with advanced prostate cancer.
Is early diagnosis a significant factor in the treatment of prostate cancer? Should screening be more widely available?
Prostate cancer which is caught and treated early is potentially very curable. We tend to talk about clinically significant cancers, which refers to cancers which actively need to be treated; and the earlier a clinically significant cancer can be caught, the better the chance for capturing it and getting rid of that cancer completely.
There is no prostate cancer screening programme at the moment in the UK. Currently, the best first test that we have is the prostate-specific antigen (PSA) blood test. PSA is a protein expressed by normal prostate cells, and if a blood test shows a rise in PSA all it indicates is that a man may have a prostate problem – it doesn’t tell you what that problem is, but it is a trigger for more specific clinical investigations. The majority of men who have raised PSA levels are not found to have prostate cancer, while there are a smaller number of men whose PSA levels will not go up even if they do have prostate cancer, so the PSA test is not felt to be good enough for a screening programme.
The risk of prostate cancer increases with age. In the UK there is a pragmatic approach, whereby any man over the age of 50 or any man over the age of 45 who is in a high-risk group – black men and men with a family history of prostate cancer – is entitled to have a PSA test once they have had a chat with their GP to understand the limitations of the test. If a man were interested in being tested, he would first have a chat with his GP: it is likely that the GP would perform a PSA test; and they may also do a digital rectal examination. By inserting a finger into the rectum, they can sweep the back part of the prostate, both to get an idea of any changes in size but also to see if there are any obvious lumps or bumps or changes in texture. If anything abnormal is there, that would also trigger an appointment at the hospital.
There was a trial conducted at Imperial College London investigating the relative benefits of a fast MRI scan in prostate cancer screening and examining whether that could be used to develop a screening programme similar to women having mammograms to screen for breast cancer. This study, Prostagram, showed that having these MRI scans picks up more significant prostate cancer. The initial study had just over 400 subjects and they are looking to do a much bigger trial with around 20,000 men to determine whether this option would potentially be feasible in the future as a screening programme, but that research will be dependent on their getting additional funding. There is hope out there – a lot of research is going on internationally to try and find something good enough to implement into a proper screening programme.
What are the key risk factors? What preventive or protective measures can be taken to lessen the risk of the disease?
Those most at risk of prostate cancer are men over 50, black men over 45, and men with a family history of prostate cancer. We also know that men who are overweight are more likely to develop a more aggressive type of prostate cancer. The advice that we give is simply to eat a healthy diet – a diet which is good for the heart is probably also good for the prostate – stay active and try and stay at a healthy weight.
What support does Prostate Cancer UK offer for patients and healthcare providers?
We have a team of Specialist Nurses who provide support and information which is based in clinical evidence: we do that by telephone, email, live chat and social media; the Specialist Nurses took over 12,200 contacts between April 2020 and March 2021. The charity also produces a great deal of written information, which is superbly written by a brilliant team; we have a sizeable section on our website aimed at health professionals, which includes free learning; and we fund a lot of research. We have a risk checker on our website; men can answer a few questions and within 30 seconds, it will tell them if they are in one of the higher-risk groups. There is also a policy team so if a proven new medication or procedure becomes available, they will work to get it through the approval process.

There are a number of prostate cancer support groups which people can access through the charity. We also have a ‘one-to-one’ service, which enables men to talk with other men who have been through a similar treatment pathway: sometimes men who are diagnosed with prostate cancer are given a choice of three or four treatments, and this service can help them to navigate which is the right one for them. Hormone therapy often causes a lot of fatigue in men, so we have a fatigue service which looks at trying to maximise energy levels. We also have a sexual support service, because the erectile nerves pass very close to the prostate, meaning that a lot of treatments can affect erectile function. This is something that men are not really given enough time to talk about, so we have colleagues who have a specific interest in that and men can book themselves in on our website and arrange a phone call with somebody who has a specific interest in sexual support.
How has the COVID-19 pandemic affected the diagnosis and treatment of prostate cancer in the UK?
When the pandemic first hit we heard from quite a lot of people who were in distress, because some of the workforce was being moved quite rapidly; and so people who had been diagnosed with prostate cancer suddenly found that their clinical support network was no longer there. Early on in the pandemic, we were also hearing about people who were having their treatments delayed and they were essentially left in limbo. It did get better through the year: we did hear a lot from men who were feeling bewildered and anxious at the beginning of COVID-19, but more recently, the calls that we have been taking have been gradually getting back to normal; the NHS has tried to pull out all the stops to get diagnostic tests and treatments back on track. We are still hearing that surgery is being delayed in some regions across the UK – that depends partly on how busy local hospitals are with COVID-19 cases.
Have any new developments or innovations improved the success rate of treatment in recent years?
There are a number of ongoing clinical trials across the UK. Precision medicine is an evolving area in prostate cancer treatment. These are drugs that work for particular cancer mutations. One of the first of these is Olaparib.
Imaging has greatly improved in recent years. When I started in 2015, men with suspected prostate issues would go to the hospital and the first test they would have done would be a biopsy, then later on, those who were found to have some cancerous cells would then have a scan – but you would have to let the bruising from the biopsy subside before you did the scan. Now hospitals have more sophisticated MRI scans; and that is the first test that men will have. A radiologist can use those scans to determine the likelihood that a man might have cancer. This means those men who have might have an abnormality but who present a very low risk of prostate cancer may avoid unnecessary biopsies. It compresses the amount of time between scan and biopsy and speeds up the diagnostic process.

Men with metastatic prostate cancer have a sequence of treatments available. Historically, some treatments were used only when a man’s hormone therapy stopped controlling the cancer completely. Over the last few years research has demonstrated that giving some of these treatments, such as docetaxel chemotherapy or abiraterone, earlier on can benefit men and improve outcomes. This has become standard practice and men will often have these treatments within 12 weeks of starting their hormone therapy.
There is also a new type of scan called PSMA PET scanning. The radioactive tracer used for this scan includes a molecule which can attach to the proteins on prostate cancer cells, and that makes them show up on a scan. These scans may be better at detecting small amounts of cancer outside the prostate than more traditional scans, especially when PSA levels are relatively low. Research is ongoing to try and find the best way to use this information to improve treatments for men. In addition to the diagnostic potential offered by the PSMA PET scan, researchers are now also looking at the possibility of attaching therapeutic agents to those molecules which bind to the prostate cancer cell receptors, as a potential means of treatment.
Prostate Cancer UK’s 30-second online risk checker is available at prostatecanceruk.org/riskchecker. Anyone with concerns about prostate cancer can contact Prostate Cancer UK’s Specialist Nurses on 0800 074 8383 or online at www.prostatecanceruk.org.
Emma Craske
Senior Specialist Nurse
Prostate Cancer UK
+44 (0)800 074 8383
https://prostatecanceruk.org/
This article is from issue 17 of Health Europa. Click here to get your free subscription today.







