Walter and Eliza Hall Institute of Medical Research (WEHI) researchers have identified an enzyme that is essential for immune T cells to correctly identify threats that reduce the risk of autoimmune disorders.
The enzyme was discovered in the thymus, an important organ where immune T cells learn to fight infection. The new findings revealed that the enzyme KAT7 is necessary to activate thousands of genes required for ‘training’ immune T cells not to attack healthy tissue. Without proper training, immune T cells are at risk of sabotaging the immune system, which could lead to autoimmune disorders such as type 1 diabetes or multiple sclerosis.
The findings, published in Science Immunology, paves the way for potential treatments to target KAT7, which could modify the training of immune T cells, reducing the chance of autoimmune disorders developing.
The research was led by former WEHI PhD student Dr Melanie Heinlein, along with Associate Professor Tim Thomas and Associate Professor Daniel Gray from WEHI, in collaboration with researchers at Monash University and the Weizmann Institute of Science in Israel.
Training immune T cells
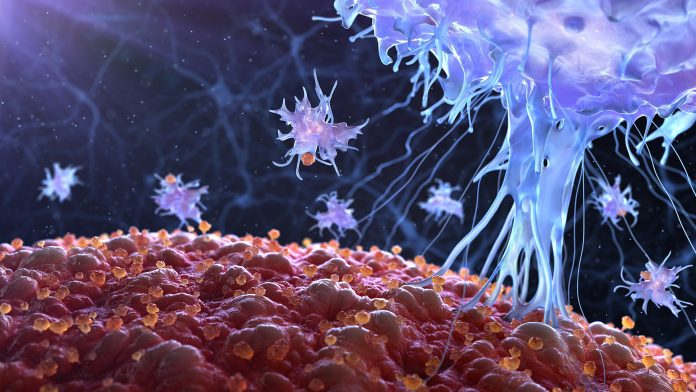
Immune T cells are trained to identify and fight pathogens and taught not to attack healthy organs in the thymus. To prepare, immune T cells are shown a ‘preview’ of all the various components of healthy tissues they could encounter once they exit the thymus.
Whilst it was previously known that the Autoimmune Regulator (AIRE) protein activated the thousands of genes needed for this preview, it was unclear how AIRE knew which genes it needed to ‘switch on’, until now.
Dr Melanie Heinlein said the new findings revealed that the enzyme KAT7 was crucial for determining which genes AIRE needed to activate for immune T cells to be properly trained.
She commented: “Like a training coordinator, KAT7 directs AIRE to the thousands of genes that must be activated for the ‘boot camp’ to run smoothly. KAT7 does this by tagging the genes that AIRE needs to ‘switch on’ for the preview of the body’s proteins to work. When all goes to plan, immune T cells are trained not to fight any normal tissues they could encounter in the body, ensuring they do not cause autoimmune disorders.”
Importance of KAT7
Associate Professor Tim Thomas said KAT7’s crucial role in keeping immune T cells to task was made clear when the researchers used a new drug to block its function. Thymus cells making AIRE educate the surrounding developing T cells.
“We showed how a KAT7 inhibitor, developed in collaboration with Jonathan Baell at Monash University, was able to stop AIRE from switching on the genes needed to properly train immune T cells. Stopping this process sent the immune system into overdrive, leading to immune T cells going rogue and causing a range of autoimmune conditions in pre-clinical models. This shows a clear link between KAT7 and AIRE in maintaining immune tolerance,” he said.
“This has been a wonderful team effort. The highly collaborative study was made possible with expertise from across WEHI’s Flow Cytometry Laboratory, Genomics Facility, and the Centre for Dynamic Imaging, along with colleagues from Monash University and the Weizmann Institute of Science in Israel.”
Treatment potential for autoimmune disorders
Autoimmune disorders result from a dysfunction of the immune system, attacking healthy cells, tissues, and organs. However, the researchers said the discovery could lead to new treatments for restraining immune T cells to prevent autoimmune disorders, or for supercharging immune T cells to fight disease.
Associate Professor Daniel Gray commented: “Our research shows KAT7 could be targeted to modify the training of immune T cells so they can either be stopped from causing autoimmunity or boosted to fight disease.
“Potential applications of this knowledge include organ-specific autoimmune diseases such as Type 1 diabetes and multiple sclerosis, as well as cancer immunotherapy. In the latter scenario, the immune system could be supercharged to combat cancer by blocking KAT7 in the thymus.”









