
Following the first real-world study which examined the reduction of HAIs using air cleaning systems, Air Purity explains how its adaptive, next-generation disinfection units are improving indoor air quality and patient outcomes.
The air disinfection system designed by Air Purity sets out to demonstrate significant reductions in respiratory illness through airborne infection within clinically vulnerable wards. This involved a world-first study, conducted in a real-world environment, and learnings are increasingly shared with other NHS trusts.
CEO of Air Purity and developer of the AeroTitan and AeroSentinel systems, Darren Sloof, explains why these systems in particular were selected for use in the study to pragmatically assess both the challenges and possibilities of showing real-world airborne infection reduction through means of airborne mitigation.

What prompted the idea to develop the Air Purity System?
Increasing infection statistics pre-COVID meant that, theoretically, there was more happening than current guidelines account for. We looked at how transmission could occur through fluid dynamic principles; it was necessary to build a new type of system to ensure that if a noticeable positive change to infections were to happen it was given the best chance when applied in a clinically complex patient area.
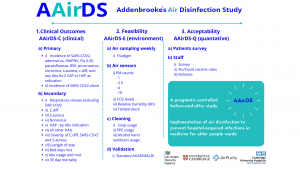
Can you tell us about the Addenbrookes Air Disinfection Study (AAirDS)?
The initial study started in an elderly care ward in September 2021 and has run for 12 months within Cambridge University Hospitals. It investigates whether airborne infection reduction through airborne intervention is achievable and if there is any correlation between environmental factors and infections.
Working with Cambridge University Hospitals for a significant period of time prior to the study ensured the best possible technology development and chance of success. This warranted we meet the study requirements and have UKHSA funding approval. The technology and commissioning were novel, as is the study, so we are breaking new ground in better understanding infectious disease outbreaks.
How is the system being used in the Addenbrookes Air Disinfection Study?
The Air Purity system is a combination of AeroTitans (air disinfection units) and AeroSentinels (air quality sensors).AeroSentinels are used for the commissioning process and can actively assess how aerosols move, and where potential risks could arise. The technology continues to be developed through learning outcomes but has been a big part of facilitating the improvement of results.
AeroTitans are devices that control and manipulate the ward’s environment, cleaning at very high rates (10+ air changes per hour), and preventing ward outbreaks. They communicate within a network to ensure minimal disruption to patients and staff without any physical intervention or controls needed.
Why is the study duration 12 months specifically?
We need to factor in seasonality and how it impacts the environment and types of infections. Most airborne infection outbreaks seem to be cyclical; over a duration of time, we can show trends and aim to eventually statistical relevance. AAirDS has expanded into other trusts, as we implement devices into new environments and clinical groups, the more we learn.
This type of study will unlikely be replicated again. Our goal is to both answer and generate future questions in full transparency and efficacy. This will be key to driving systematic change and further developments, both scientifically and commercially, within airborne infection prevention and also non-healthcare environments.
What has the study shown so far?
Planning and commissioning are key to yielding success in potential airborne infection reduction. Ventilation is carefully planned, and air disinfection systems should be treated at the same level. Testimonials from the wards over the first 12-month segment give a compelling and honest view so far.
Results will likely be published in May 2023, although extension studies are taking place even now, so it will be a continual learning curve. The publication will certainly provide a strong benchmark for a decrease in infections with COVID being the proxy, as this is the most prevalent and coveted.

Is there a correlation between airborne infection and environmental data (Indoor Air Quality)?
We can see a correlation between better air quality and noticeable reductions, however, we cannot yet ascertain if it will have statistical relevance. A good way to look at indoor air quality is to first understand the risks imposed on an individual if the air quality is perceived as bad, and what you are looking to achieve.
Poor air quality can have metrics to define better from worse, nevertheless, exposure duration will present a higher risk factor.
Being exposed to bad air quality for a moment, versus days of moderate air quality, which is worse? We need to be honest and say we cannot know as we are still understanding or coming to terms with modes of transmission. What we do know is focusing on how the air moves within an environment and how we control this, is critical to removing the biodiversity and ensuring infection stays localised to prevent outbreaks.
What does the installation tackle?
We are seeing very positive results in infection reductions with Sars-CoV-2 being the proxy, but we know more types of infections are patient-to-patient and the key mode of travel is via air. Nonetheless, this does not mean it is necessarily the mode of infection transmission. The installation is there to tackle any environment but predominantly focuses on non-ventilated or poorly ventilated spaces. The setup will control the environment meaning fast mixing, diluting, and cleaning are achieved with a minimum target of ten air changes per hour (ACH).
Implementing any intervention within the ward is challenging. How do you overcome this?
There are multiple steps needed to overcome barriers to successful intervention. Firstly, educating both patients and staff on what we are trying to achieve and making the invisible visible by offering materials and understanding the spaces and limitations. One of the key issues in hospitals, and other areas, is normally the limitation of plugs and space, any system implemented needs to be tailored to that environment if you are serious about tackling infections.
Service capacity is also incredibly important – how are the systems being maintained? Who manages this?
We have learned a lot over the last three years but continually the ability to change and adapt must be there to facilitate different types of environments and clinical groups. Engaging with staff from the very beginning and along the way has provided significant understanding for everyone involved.
Steps of engagement to join the study or look at an air disinfection implementation?
Contact Air Purity directly. While our central research partner is Cambridge University Hospitals and UKHSA, contractually we can enable countless extension studies or help mitigate outbreaks. Or for more information please visit www.aairds.com, there you can find videos and more literature.
How many NHS trusts are adopting the study or system?
The first 12 months of study are complete and validated and we are now moving into other trusts. Currently, we have nine more trusts starting the commissioning stage at the end of this year, with a realistic expectation of over 100 trusts by 2023.
What is the ultimate outcome for AAirDS?
To bridge engineering and infection prevention, generating an acceptance of better ways to deal with both pandemics and other infections. Results next year will be a catalyst to drive further funding and studies, and also enable us to look at ways to utilise technology for the greater good of both patients and staff.

Junior Sister Elderly Care
Cambridge University Hospitals

Interim Senior Sister Ward G6
Cambridge University Hospitals
Thoughts from staff within the settings of the AAirDS
“From an infection point of view, it has been highly beneficial for the ward, both patients, staff, and visitations. During the Air Purity intervention, we noticed drastically reduced cases of C-diff, MRSA, Norovirus, and influenza. We see a noticeable change in reductions in our common infections such as UTIs as well. It is evident we are no longer closing bays or wards, the system is highly beneficial to save cost and improve the health of all occupants.”
“The study with Air Purity has been in the ward for the last 12 months. Patient relatives were very happy as they can see that the hospital is actively trying to find ways to keep patients safe, especially when it first started, COVID was still a primary cause of concern. Our patients are elderly and some of them are confused. Initially, some of them thought it was a mailbox, but it did not further add to their confusion as it was eventually not emitting much noise.
“We feel that since the study started, we did not have as many outbreaks particularly respiratory type e.g. flu or COVID. I have been working in the ward for the last eight years and I can always expect that in a year we would always have a respiratory virus, such as flu outbreak, as our ward layout does not have doors on bays and only fire doors to divide the ward into three sections. It has really made a big difference based on my observation.”
Darren Sloof
Air Purity ltd
This article is from issue 23 of Health Europa Quarterly. Click here to get your free subscription today.









