Surface Medical highlights the risks posed by damaged hospital mattresses, and how a simple patch can create a safer hospital environment while saving healthcare facilities money.
Despite the presence of infection prevention and control programmes which have been in place since the 1950s, and hand hygiene protocols which been in place for over 100 years, healthcare-associated infections (HAIs) – infections patients acquire when receiving treatment for other conditions – continue to be a widespread and costly issue for healthcare systems. In the USA alone the Centers for Disease Control and Prevention (CDC) estimates that HAIs account for an estimated 1.7 million infections and 99,000 associated deaths every year. Globally these same statistics are astonishing, with costs in the tens of billions.
To reduce the rate of infection, tremendous attention is paid to the cleaning and disinfection of surfaces in patient rooms and the decontamination of medical equipment and devices. Studies have demonstrated that patient mattresses are one of the highest touch points in hospitals and can harbour dangerous pathogens1 that result in the transmission of infection and, in some cases, patient death. Damaged hospital mattress covers are particularly concerning because of their proximity to patients.2
How did Surface Medical get started?
The Surface Medical story began when a Canadian chiropractor, Dr Jeffrey Schacter, expressed frustration to one of his long time patients over a costly and troublesome problem. Dr Schacter was frustrated because, after many years of looking, he could not find an easy and effective repair product for the vinyl upholstery on his treatment tables. The day he complained about this problem to his patient was the day after his treatment tables were reupholstered, and another patient had inadvertently punctured the vinyl upholstery on one table with his belt buckle. Dr Schacter had been in practice for more than two decades and knew damaged treatment surfaces presented as unprofessional and unhygienic – an embarrassing problem to have.
As it happens, the patient was part of a healthcare consulting group which quickly recognised that compromised treatment surfaces are much more prevalent, and much more dangerous, in hospital settings. This consulting group included a nurse with 25 years’ frontline experience, Barbara Potter. She rightly conjectured that damaged soft surfaces in hospital rooms would present an even greater problem: damaged surfaces could pose a risk to patient safety and the safety of healthcare workers through occupational exposure. It was because of this realisation that Surface Medical’s founding team, Fabrizio Chiacchia and Iwain Lam, determined to develop a simple, practical and affordable solution to the problem of damaged mattresses; and, after more than two years of research and development, CleanPatch was born.
The problem of damaged mattresses
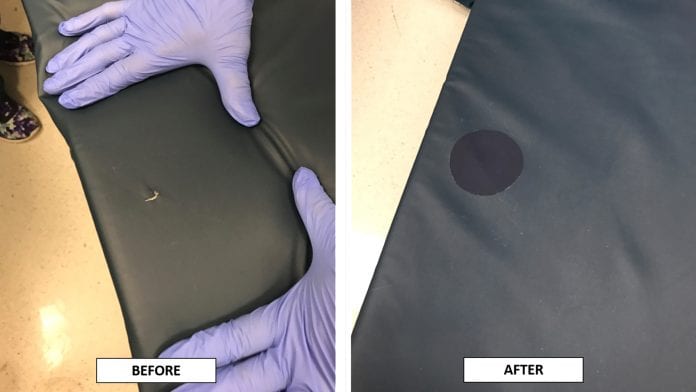
Soft surfaces such as hospital mattress covers, stretchers, and other high-touch clinical equipment are prone to damage from daily wear and tear as well as damage produced by harsh chemical cleaning agents and sharp objects such as needles. Once a mattress surface is compromised, it cannot be properly disinfected no matter what type of cleaning agent is used.
Mattress covers are routinely damaged at a rate of 25% to 45%, putting patients and frontline workers at a greater risk of infection which can be avoided if damage is quickly addressed. Mattress covers should be examined regularly for visible signs of damage and permeability: staining to the exterior of the mattress cover may indicate fluid penetration of the inner core and possible contamination. Once they are damaged, mattress covers are no longer impermeable to fluids and are a potential source of HAI contamination.3 Studies also show that restoring the mattress surface to an intact and impermeable state allows for proper disinfection and is a key factor in outbreak control.
Past practices dictated that once a surface was damaged, the only approved solution was to replace the entire mattress, which is expensive and generates biohazardous waste. Sadly, due to budgetary constraints and the risk of reducing the number of available hospital beds by taking equipment out of service, hospital staff will often resort to applying unapproved products such as commercial tape or wound care dressing; or worse yet, staff may opt to ignore damaged mattresses for lack of an expedient and economical solution and, in doing so, potentially expose patients to pathogens through cross contamination. Both the UK National Health Service (NHS) and US Food and Drug Administration (FDA) have issued safety communications on the problem of damaged mattress covers and the associated risk of cross contamination among patients. From 2011 through 2016, the FDA received over 700 reports of a damaged hospital bed mattress cover failing to prevent blood or body fluids from leaking into the mattress core.
How was CleanPatch developed?
CleanPatch was created with three key objectives in mind:
- To create a repair solution that is easy to apply;
- To provide material amounts of cost savings for healthcare facilities; and
- To improve patient safety by creating a cleanable, intact surface.
Unlike an off-the-shelf repair tape, CleanPatch had to be durable enough to remain fully adhered to the mattress surface despite frequent exposure to aggressive chemical cleaning agents such as accelerated hydrogen peroxide, bleach, isopropanol, and quaternary ammonium. It was also imperative that CleanPatch be non-cytotoxic and hypoallergenic, and sufficiently durable to withstand rigorous clinical use4.
CleanPatch was created through testing at the University of Calgary and in close collaboration with a hospital research centre, frontline healthcare workers, infection control practitioners and independent testing facilities. After several years of laboratory testing and clinical validation testing, CleanPatch was commercially launched in 2013 as a registered Class 1 Medical Device, and its innovation and technology have since been recognised globally.
What is CleanPatch?
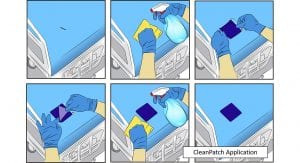
CleanPatch is, essentially, a simple peel-and-stick medical repair patch. The concept behind the product, which everyone can relate to, is like applying a bandage over a wound: when damage is identified, the site is assessed prior to application. If repair is appropriate, CleanPatch may then be applied over the damage site after the surface has been cleaned. When applied appropriately, the repaired surface is impermeable and ready for use. What makes CleanPatch unique is that it is the only Health Canada, FDA, and CE mark-registered medical device designed to repair damaged soft surfaces; it empowers hospital staff to repair equipment quickly and effectively without compromising patient safety.

How did the markets react to CleanPatch?
Surface Medical has received widespread recognition for this innovative repair solution. In 2014, it was recognised by the ASTech Foundation for Outstanding Science and Technology, for its commitment to healthcare innovation and for contributing to the medical technology industry in our community. In 2015 Chiacchia and Lam were awarded the prestigious Ernest C Manning Innovation Award for developing and commercialising CleanPatch, and in 2016 Surface Medical’s fast growth earned it the Global Entrepreneurship Award from Startup Canada.
CleanPatch has been adopted by thousands of healthcare facilities in over fifteen countries including acute and long term care facilities, professional health practices such as chiropractic and physiotherapy clinics, and patient transport services. In recent years, Surface Medical has produced two new repair products for healthcare surfaces: CleanPatch-V for the repair of damaged vinyl upholstery such as wheelchairs, commodes and exam tables, and CleanPatch-P for the repair of gel pad positioners. Taken together, the CleanPatch product line can address damage in over 90% of all soft surfaces commonly found in healthcare facilities.
What are some of the biggest challenges to adoption?
Because CleanPatch is a market-first offering, the biggest challenges have been education and implementation. Prior to the introduction of CleanPatch, the only option open to healthcare facilities was to remove damaged equipment from service because facility guidelines did not have access to a validated soft surface repair product. As a result, Surface Medical has made significant effort to advise healthcare facilities that equipment replacement can be avoided by using CleanPatch to repair minor damage.
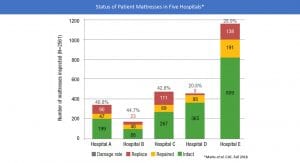
In 2018, a peer reviewed study was published in the Canadian Journal of Infection5. Surface Medical worked with five leading Canadian hospitals to assess more than 2,500 patient mattresses: it was found that 32.5% of patient mattresses were damaged. 55.6% of damaged mattresses did not show signs of moisture penetration and were successfully repaired with CleanPatch. The study highlighted the prevalence of damaged surfaces in hospital settings and the risk they pose to patients. It also demonstrated that more education is required to increase clinician and staff awareness of this issue. Fortunately, CleanPatch has been well received by the healthcare community as a repair solution, and guidelines and protocols are being updated to reflect this option as an approved alternative to equipment replacement. A significant policy change came in 2018 when the Joint Commission amended its guidelines on environmental cleaning to condone patching damaged surfaces when the repair is performed with an approved and validated repair product.6
What are some surprises that happened along the way?
Since market launch, CleanPatch has proven to be more versatile than its creators originally imagined. In addition to healthcare facilities, CleanPatch has also been used by military facilities in the far North, where infection risk is high and equipment replacement is difficult; it is also stocked on ambulances so stretcher mattresses can be repaired on the road; and it has been used to repair beds in congregate living facilities such as homeless shelters. Along the way, Surface Medical has developed partnerships with disinfectant manufacturers and hospital mattress manufacturers in a united front to support more comprehensive environmental hygiene protocols.
Has the COVID-19 pandemic affected Surface Medical?
The novel coronavirus outbreak has created an unprecedented situation globally, and it has put a brighter spotlight on the importance of environmental hygiene as a means to combat the transmission of viruses and pathogens. It is important now more than ever to ensure the consistent application of good hygiene practices in healthcare facilities, and it is clear that hospitals are actively looking for innovative products that can be used to enhance their infection prevention protocols. A recent publication shows that frontline healthcare workers are at greater risk for contracting COVID-19 than the general community, even when personal protective equipment is used scrupulously.7
This represents a major opportunity for CleanPatch implementation, as many healthcare facilities around the globe revisit their cleaning processes to identify gaps in their infection control protocols. With the added budgetary pressure created by increased spending on personal protective equipment and other critical lifesaving equipment, the implementation of CleanPatch is proving to be a valuable and welcome addition to environmental hygiene protocols. Surface Medical is working closely with its partners, healthcare associations, and policy makers to increase product awareness as healthcare systems around the world strive to enhance their infection control practices.
What’s next for Surface Medical and CleanPatch?
Looking ahead, Surface Medical aims to expand its geographical footprint worldwide and to build CleanPatch into a truly global brand by broadening its partnership and distribution network, and thereby increase its reach. Our immediate strategic focus is to expand CleanPatch distribution into Eastern Europe as well as Asia and the Middle East. Surface Medical will also continue to work behind the scenes to create simple, innovative, cost effective products that support environmental hygiene practices.
References
- Huslage et al. Infection Control and Hospital Epidemiology. 2010. 31 (8) pp. 850.
- Creamer, E. and Humphreys, H. Journal of Hospital Infection 2008 69, 8-23.
- Bradbury, S. et al. American Journal of Infection Control. April 2014, 42(4). P.421–422.
- Wong et al. Canadian Journal of Infection Control. Fall 2015. 30(3). P.165-170.
- Marks et al. Canadian Journal of Infection Control. Fall 2018, 33(3) p.171-175.
- Joint Commission Resources, Environmental Infection Prevention: Guidance for Continuously Maintaining a Safe Patient Care and Survey-Ready Environment, 2018
- Nguyen, L.H. et al. medRxiv. May 2020. Risk of COVID-19 among frontline healthcare workers and the general community: a prospective cohort study
Iwain Lam
President/CEO
Surface Medical Inc.
+1 403 383 7800
iwain@surfacemedical.ca
www.cleanpatch.ca
This article is from issue 14 of Health Europa. Click here to get your free subscription today.










