US researchers have created a cutting-edge smartphone app that accurately calculates an individual’s genetic risk for coronary artery disease (CAD).
Developed by a Scripps Research team, the innovative app not only estimates the users’ risk for coronary artery disease but has also shown in a study to influence high-risk individuals to seek out appropriate medication after utilising the app.
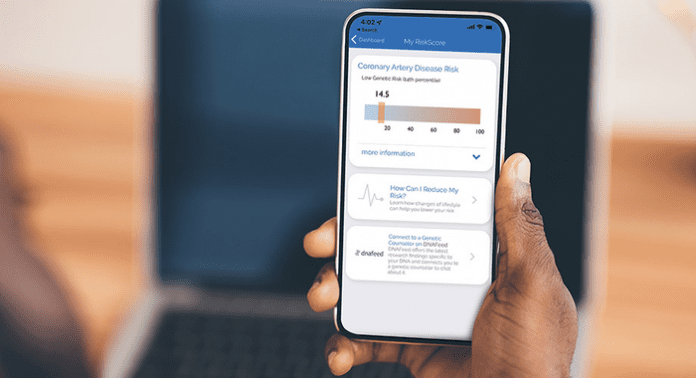
The smartphone app – called MyGeneRank – inputs a users’ genetic information from the 23andMe genetic testing company, from which it creates a CAD risk score based on the DNA data. The team conducted a study including 721 participants, finding that those with high-risk scores were more likely to start using statins or other therapies that reduce cholesterol than those with low-risk scores.
Ali Torkamani, PhD, the senior author of the study and a professor and director of Genomics and Genome Informatics at the Scripps Research Translational Institute, said: “We saw about twice the rate of statin initiation in the high genetic risk group vs the low genetic risk group, which indicates that strategies like this could make a big contribution to public health—heart disease being the largest cause of death globally.”
The team’s study is published in npj Digital Medicine.
Prevalence of coronary artery disease
Estimates from the US Centers for Disease Control and Prevention suggest that 18 million adults in the US alone have coronary artery disease, the most common type of heart disease, with more than 300,000 Americans dying of heart attacks annually. CAD is characterised by the hardening and narrowing of the arteries that feed the heart.
The burden of coronary artery disease has been alleviated over the last 20 years due to the implementation of statins, such as atorvastatin and simvastatin, and other non-statin medications that lower bloodstream levels of cholesterol and other fat-related molecules called lipids.
However, researchers estimate that nearly 50% of men and 10% of women in the US aged between 45 and 65 years are at least at intermediate risk of CAD, with only around a third using lipid-lowering drugs. Now, experts suggest that smartphone apps may be an efficient and effective method for informing those at a high risk of CAD, enabling them to seek appropriate medical advice and treatment for their condition.
Evan Muse, MD, PhD, the first author of the study and a cardiologist and lead for cardiovascular genomics at the Scripps Research Translational Institute, said: “We now have the opportunity to integrate a person’s genetics into their cardiovascular health assessment to help them better understand their individualised risk and empower them to make the necessary modifications – including the addition of statin therapy – to their risk factor optimisation plans.”
Torkamani added: “Even if someone finds out they have a low genetic risk for CAD, knowing their score can help—for example, if they also know they have high risk overall, that may suggest other non-genetic factors like lifestyle are contributing to their risk and that they should consider making changes.”
The MyGeneRank app
MyGeneRank is available on iPhone andAndroid. Once downloaded, users link their 23andMe data and complete consent forms and health-rated surveys that include questions about the use of lipid-lowering drugs. Subsequently, the app uses this data to generate a risk score for coronary artery disease based on the latest recognised genetic risk factors. The app will then follow up one year later with questions about the users’ current lipid-lowering medication use.
The team promoted the app at scientific conferences and through social media advertising campaigns, enrolling 3,800 eligible respondents, of which 721 provided enough data for the analysis. The results demonstrated that those who were not taking lipid-lowering medication at the study’s inception but were informed of their high gene-based risk scores for coronary artery disease were twice more likely to start therapy than those with low-risk scores.
Compared to those in the low-risk category, the participants in the high-risk were 1.4 times more likely at follow-up to report the use of a statin lipid-lowering drug, and around four times more likely to report the use of a non-statin lipid-lowering drug. High-risk respondents also started lipid-lowering treatment much earlier – age 52 on average – compared to 65 for the low-risk group.
“On the whole, it looks like a significant effect, especially considering that we were giving respondents only appropriately contextualised information about their gene-based risk scores—we weren’t directly telling them to go out and start taking medications,” Torkamani said.
The team is now planning to investigate more extensive and longer-term studies of coronary artery disease risk, including clinicians, and recording differences in cardiovascular health outcomes, such as heart attacks.







