MedUni Vienna researchers have discovered a novel technique that estimates alcohol consumption in fatty liver disease patients.
Understanding whether a patient has non-alcoholic fatty liver disease or alcohol-related fatty liver disease determines the treatment and prognosis approach. Despite this, there is no reliable tool to distinguish between the two.
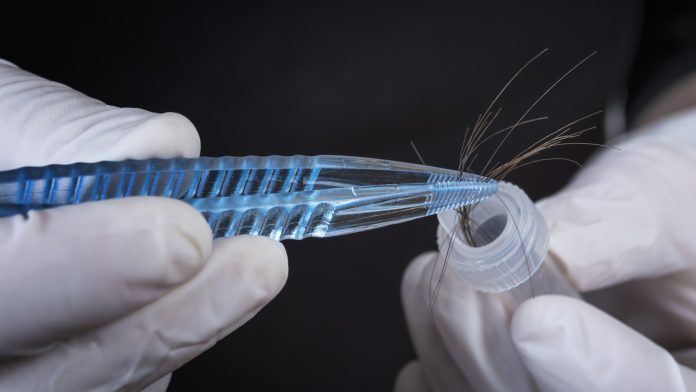
In a study by MedUni Vienna, a novel method that uses the patients’ hair can determine alcohol consumption in fatty liver disease. The researchers found that around 30% of patients with presumed non-alcoholic fatty liver disease were at risk of alcohol-related liver damage.
The research was published in the Journal of Hepatology.
Measuring alcohol consumption of fatty liver disease patients
The researchers assessed the alcohol consumption of 184 patients’ in treatment for non-alcoholic or alcohol-related fatty liver disease in clinics in Vienna and Oberndorf.
The team, led by Katharina Staufer and Michael Trauner, Head of the Division of Gastroenterology and Hepatology at MedUni Vienna and University Hospital Vienna, evaluated currently available methods of alcohol detection against the novel method. This involves combining the alcohol parameters ethyl glucuronide in hair (hEtG) and urine (uEtG) with the AUDIT-C (Alcohol Use Disorders Identification Test) questionnaire. The novel method detects alcohol consumption in 29% of patients with alcohol-related liver disease and presumed non-alcoholic fatty liver.
Medical research has yet to provide clear evidence of alcohol’s impact on fatty liver disease. Recent studies have found that patients consuming an equivalent of 1.5 litres of beer can develop serious sequelae such as liver scarring.
The impact of patients underestimating their alcohol intake
The stigma surrounding alcohol consumption causes discrepancies in early fatty liver disease diagnosis. Patients will often underestimate or fail to report their alcohol intake because they are afraid of judgement, have an alcohol use disorder or generally miscalculate their consumption.
“Measuring ethyl glucuronide in hair and urine in addition to using the AUDIT-C questionnaire can help to determine alcohol consumption and thus, for the first time, enable a frank conversation about actual alcohol consumption and its consequential damage,” explained lead author Katharina Staufer, stressing the importance of a trusting doctor-patient relationship.
In the last two decades, experts have proposed changing the name of non-alcoholic fatty liver disease to “metabolic dysfunction-associated fatty liver disease” (MAFLD). “The results of our study are a further step towards improved diagnostic criteria for fatty liver disease,” concluded Michael Trauner.









