Researchers from the University of Pennsylvania (Penn) have developed a new method to cut manufacturing time for CAR T cell therapy.
The cell manufacturing process for CAR T cell therapy, which was researched and developed by Penn, typically takes nine to 14 days. However, in the pre-clinical study, scientists were able to reduce the processing time and generate functional CAR T cells with enhanced anti-tumour potency in 24 hours.
The study was led by Center for Cellular Immunotherapies researchers, Michael C. Milone, MD, PhD, an Associate Professor of Pathology and Laboratory Medicine, and Saba Ghassemi, PhD, and Research Assistant Professor of Pathology and Laboratory Medicine.
The pre-clinical study was published in Nature Biomedical Engineering and was conducted by a team in the Perelman School of Medicine at Penn.
What is CAR T cell therapy?
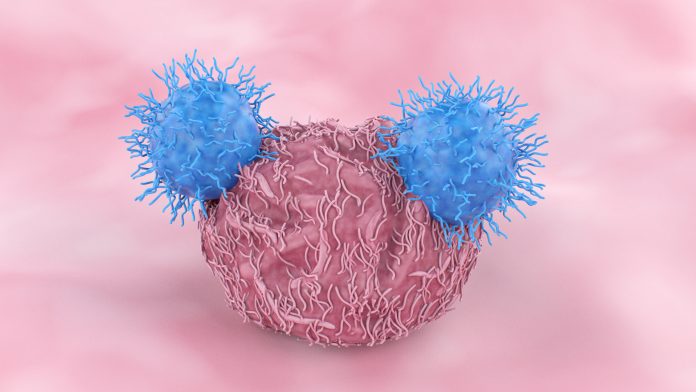
CAR T cell therapy is a type of immunotherapy utilised to fight cancer with a patient’s altered immune cells. T cells are taken from a patient’s blood and changed in the lab by adding a gene for a receptor (called a chimeric antigen receptor or CAR). The CAR T cells are then infused back into a patient to find, bind to, and destroy cancer cells.
However, when removed from the body for too long during the engineering process, T cells can lose their ability to replicate, which is a critical component in their effectiveness as a living drug. To solve this issue, the Penn research team pursued new methods to shorten the process without sacrificing the T cell potency.
Reducing the cost of manufacturing
In animal models, researchers discovered that the quality of the CAR T cell product is an important determinant of their efficacy. Their experiment provided evidence that a smaller number of high-quality CAR T cells that are generated without extensive expansion outside the body is superior to a higher number of reduced-quality CAR T cells that are extensively expanded before returning to the patient.
Traditional manufacturing approaches require T cells to be activated in order for the cells to replicate and expand in quantity. Penn researcher’s manufacturing process utilises a lentiviral vector that delivers the CAR gene to the T cells. Lentiviral vectors, which are derived from the human immunodeficiency virus (HIV), can transfer genes like the CAR to cells without the need for this initial ’activation’ step, but this process is low in efficiency.
Penn researchers utilised their knowledge of how HIV naturally infects T cells to develop a way to overcome the requirement for T cell activation and deliver genes directly to non-activated T cells freshly isolated from the blood. This approach posed a dual benefit by expediting the overall manufacturing process, whilst also maintaining T cell potency. Patients are not being infected with HIV through this process.
Additionally, the process of engineering T cells is costly and time-extensive since the CAR T cell therapy must be manufactured for each patient. The team hopes that cutting manufacturing time could make the therapy more cost-effective and accessible to more patients. These results demonstrate the potential for a vast reduction in the time, materials, and labour that is required to generate CAR T cells, which could be especially beneficial in patients with rapidly progressive diseases and resource-poor healthcare environments.
“This innovative approach is remarkable in that it may be able to help patients who might otherwise not be able to benefit from CAR T cell therapy, such as those with rapidly progressing cancer due to significant time currently needed to generate these therapies,” Ghassemi concluded.
“Efficient reprogramming of T cells with a CAR in as little as 24 hours in a more simplified manufacturing process without T cell activation or extensive culture outside the body also offers the possibility of expanding where and when these therapies are produced.
“Not only might it improve the production capacity of centralised manufacturing facilities, but if simple and consistent enough, it might be possible to produce these therapies locally near the patient, which could be tantamount to addressing the many logistical challenges that impede the delivery of this effective therapy, especially in resource-poor environments.”
This study is a catalyst for more clinical research to investigate how the engineered CAR T cells, through this shortened approach, work in patients with specific cancers.









