NIH-funded study found that a type of magnetic resonance imaging, called neuromelanin-sensitive MRI (NM-MRI) is a potential biomarker for psychosis.
Neuromelanin-sensitive MRI signal was found to be an indicator of dopamine function in individuals with schizophrenia and an indicator of the severity of psychotic symptoms in people with this mental illness. The study, funded by the National Institute of Mental Health (NIMH), part of the National Institutes of Health, appears in the Proceedings of the National Academy of Science.
Let’s talk neuromelanin-sensitive MRI
Joshua A. Gordon, M.D., Ph.D., director of NIMH, explains: “Disturbances affecting the neurotransmitter dopamine are associated with a host of mental and neurological disorders, such as schizophrenia and Parkinson’s disease.”
“Because of the role dopamine plays in these disorders, the ability to measure dopamine activity is critical for furthering our understanding of these disorders, including how to best diagnose and treat them.”
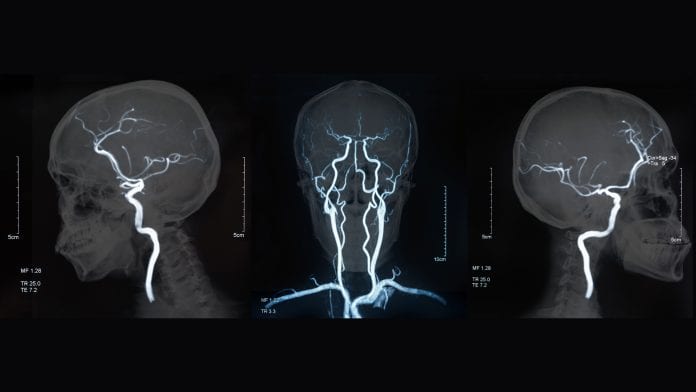
Neuromelanin is a dark pigment created within dopamine neurons of the midbrain, particularly in the substantia nigra, a brain area that plays a role in reward and movement.
Neuromelanin accumulates over the lifespan and is only cleared away from cells following cell death, as occurs in neurodegenerative disorders such as Parkinson’s disease.
Researchers have found that NM-MRI signal is lower in the substantia nigra of people with Parkinson’s disease, reflecting the cell death that occurs in these patients.
Advantages of neuromelanin-sensitive MRI
Dr. Guillermo Horga, Columbia University, USA, explains: “The main advantages of this technique are that, compared to other established and more direct measures of dopamine function, neuromelanin-sensitive MRI does not involve radiation or invasive procedures.”
“This advantage makes it more suitable for paediatric populations and for repeated scanning, which could be useful to monitor the progression of illness or response to treatment – and it only takes a short scan that could be implemented in most clinical scanners. It also affords a very high anatomical resolution compared with PET measures, which is important to examine functions or dysfunctions of specific parts of the substantia nigra.”
Detecting regional variations
To investigate the detection ability of NM-MRI, the researchers compared NM-MRI measurements of neuromelanin to chemical measurements of neuromelanin in post-mortem brain tissue. The researchers found, across all sections of tissue, that higher NM-MRI signal was associated with higher concentrations of neuromelanin.
The results confirm, for the first time, the ability of the technique to measure regional concentrations of neuromelanin. Furthermore, the results show that NM-MRI signal reflects concentrations of neuromelanin in tissue, rather than just the number of neuromelanin-containing neurons.
The researchers next sought to determine whether NM-MRI could capture variations in neuromelanin in smaller anatomical subregions within the substantia nigra. Since dopamine function is thought to differ significantly in different parts of the substantia nigra, researchers needed to determine the ability of this tool to capture these anatomical differences. So, the researchers examined NM-MRI data from patients diagnosed with Parkinson’s disease and individuals without Parkinson’s disease.
The researchers found reductions in NM-MRI signal in those with Parkinson’s disease in the lateral, posterior, and ventral areas of the substantia nigra, which are findings that correspond to the known anatomical distribution of cell loss in this brain area in Parkinson’s disease.
These results confirm that NM-MRI can capture known topographical variability within this brain structure.
A next critical step was to show a connection between NM-MRI and dopamine function. The researchers collected measurements of dopamine release capacity (as measured using positron emission tomography (PET)) and NM-MRI data from people without neurodegenerative illnesses.
Individuals with a higher NM-MRI signal had greater dopamine release capacity in the striatum (a core component of reward, motor, and cognitive systems). The researchers also found that NM-MRI signal in the substantia nigra was associated with functional MRI measures of regional cerebral blood flow.
Lastly, the researchers inspected the link between NM-MRI signal and psychosis severity, discovering that more severe symptoms of psychosis were associated with higher NM-MRI signals in the nigrostriatal pathway of individuals with schizophrenia and in those at-risk for schizophrenia.
Psychosis and NM-MRI
Psychosis is associated with dopamine system dysfunction, characterised by greater dopamine release and synthesis capacity in the striatum. The findings suggest that NM-MRI is capturing this dopamine dysfunction, supporting the role of NM-MRI as a potential biomarker for psychosis.
The findings reported in this study, taken together, validate the use of NM-MRI in populations beyond those with neurodegenerative disorders, showing it can serve as a measure of neuromelanin concentration and dopamine function in the substantia nigra.
Horga concludes: “We are now extending this work to see if we can detect abnormalities in neuromelanin signal that help us predict which individuals are more likely to develop a psychotic disorder among those who already show early symptoms of psychosis.
“We are also interested in exploring whether neuromelanin-sensitive MRI could be used in the future to determine who might best benefit from dopaminergic treatments.”









