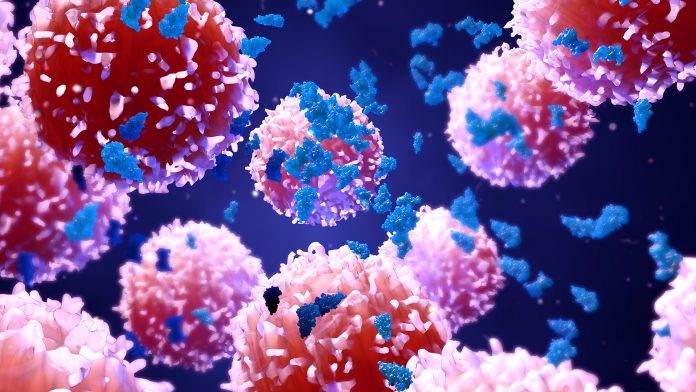
Reported in Nature Cell Biology, researchers have uncovered a use for the overlooked molecular machine in cell nucleus which could possibly hold the answers to treating aggressive leukaemia.
Many individuals forced to fight an exceptionally aggressive form of the blood cancer acute myeloid leukemia (AML) don’t survive more than five years. The only cure, a bone marrow transplant, often isn’t suitable for these patients. Now, an international team of scientists report on a long-overlooked part of a leukemic cell’s internal molecular machine called the spliceosome, where they found a hyperactive form of a protein called IRAK4 within the cell nucleus that sends cells on a cancer-causing frenzy – could this be a step towards treating aggressive leukaemia?
Breaking down the molecular machine
When the researchers targeted the hyperactive form of IRAK4 in laboratory tests to block its function in AML cells, and in-patient AML cells transplanted into immunosuppressed mice, the experimental treatment led to a significant reduction of the leukemic cells.
It also prolonged survival in the animal models, according to Daniel Starczynowski, PhD, the multi-institutional study’s senior investigator and part of the Cancer and Blood Diseases Institute at Cincinnati Children’s Hospital Medical Center, USA.
Starczynowski said that with additional preclinical research and development, the researchers would like within a few years to have their still-unnamed IRAK4 inhibitor ready for initial clinical tests in AML patients.
“There is very little we can do for these patients. Even new drugs now getting fast-tracked through the development process may only produce another six months of survival,” Starczynowski said.
“The curative option is a bone marrow transplant, but most of these patients don’t qualify. The field is really desperate for something that can help these patients.”
Sequencing in the spliceosome
Although invisible to the naked eye, the spliceosome is important. In a process of dicing and splicing, the spliceosome edits out unnecessary snippets of RNA coding called introns or exons. It then splices the loose snipped ends of RNA back together so specific proteins will do their jobs correctly.
But in AML cells, there are mutations in a gene call U2AF1, which result in RNA splicing errors. When U2AF1 functions normally, the correct snipped ends of RNA are glued back together. However, when a mutated form of U2AF1 produces incorrectly formed RNA molecules of IRAK4, it results in a version of IRAK4 protein with extra coding sequences called IRAK4-L (or long).
Together they hijack the innate immune system’s molecular processes and trigger oncogenesis in myeloid blood cells.
Can this molecular machine within the cell nucleus hold the key to treating aggressive leukaemia?
Because the preclinical results are from experiments in cell lines and mouse models, the researchers are careful to emphasise their findings may not translate clinically to human patients.
Still, the researchers say they’re encouraged to have come far enough that the design of new and potentially effective targeted cancer therapy is well underway for a blood cancer that has few such options.









