Researchers have found that liquid biopsies can detect blood cell disorders than can help identify patients at risk of blood cancer.
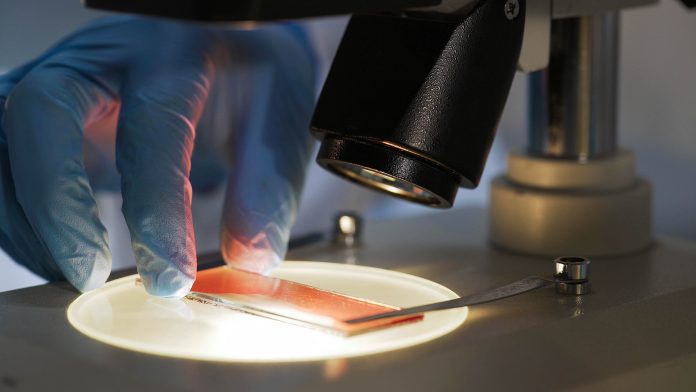
Cancer tumours release DNA into the blood, contributing to what is known as cell-free DNA (cfDNA). cfDNA can be identified through blood samples or ‘liquid biopsies’ extracted from patients. Identifying cfDNA allows doctors to better characterise cancers and select the best therapy for the patient and monitor the progression of cancer. Analysis of cfDNA can also be used to measure patients’ responses to treatment without the use of invasive biopsies taken from the tumour itself.
Clonal haematopoiesis can lead to blood cancer
Researchers from the Institut Gustave Roussy noticed that incidental discoveries of a disease called clonal haematopoiesis were common in liquid biopsies. The researchers wanted to know if they could use biopsies systematically to identify patients who have or could be at higher risk of developing forms of blood cancer, such as myelodysplastic syndrome and acute myeloid leukaemia.
Clonal haematopoiesis occurs when the haematopoietic stem cells, which can develop into different types of blood cells, begin to produce cells with a genetic mutation that is different to the genetic pattern of healthy blood cells. These cells can also release DNA into the bloodstream. Previous research has shown the risk of clonal haematopoiesis developing into blood cancer is around 1% a year, with a tenfold increase in relative risk.
The researchers examined liquid biopsies from 1,416 patients with a range of solid tumours who had enrolled in the Gustave Roussy Cancer Profiling study.
“We found that 113 patients, 8%, had at least one clonal haematopoiesis mutation that could be considered to place them at higher risk of developing blood cancers during their life,” said Dr Marco Tagliamento, medical oncologist and research fellow at the Institut Gustave Roussy.
“Out of these patients, 45 were referred to our haematology unit by their oncologist and five were subsequently diagnosed with blood cancer: one with myelomonocytic leukaemia, two with myelodysplastic syndrome and two with essential thrombocythemia” he added.
Liquid biopsies should be part of standard cancer practice
The researchers believe that finding clonal haematopoiesis in patients through liquid biopsies should trigger further haematological evaluations to reveal the risk of blood cancer in those patients.
“Early detection could prevent complications during anti-cancer treatments, for instance, alterations to blood counts, and consequent interruption or delay to treatment. It could also indicate possible diagnostic and therapeutic pathways for doctors to consider for haematological disease,” said Dr Tagliamento.
Each case was considered carefully by the Gustave Roussy Molecular Tumour Board to identify the genetic mutations involved in clonal haematopoiesis when identifying patients who should be referred for further investigation.
“Case-by-case evaluation is crucial. Different aspects must be considered when evaluating the potential impact and management of high-risk clonal haematopoiesis in patients who already have cancer. These relate, for example, to the patients, their medical history and the underlying cancers. All of them should be part of a balanced evaluation made for each individual case,” explained Dr Tagliamento.
“We will continue to apply this approach within the Gustave Roussy Molecular Tumour Board. We want to implement and improve the efficiency of the algorithm to select patients with solid cancers who could benefit from a haematological evaluation. These results are part of a team project led by Dr Mihaela Aldea and Dr Jean Baptiste Micol,” he concluded.









