Professor Michael Clark, Maureen Fallon and Professor Keith Harding, of the Welsh Wound Innovation Centre, advocate a system approach to value-based wound care.
The impact of skin and soft tissue wounds across all healthcare systems is increasingly becoming better known. Within the United Kingdom wounds consume between £4.5bn (~€5.1bn) and £5.1bn annually,1 with significant gaps in practice across the country; for example, only 16% of people with lower leg and foot wounds had an appropriate assessment of the cause of their wounds.
The Welsh Wound Innovation Centre: the first national wound healing centre worldwide
The Welsh Wound Innovation Centre (WWIC) was created in 2014 to provide leadership to wound prevention and healing in Wales. It emerged from the self-funded Wound Healing Research Unit in Cardiff University that had raised around £55m over its 24-year lifespan.
WWIC is the first national wound healing centre worldwide and has already begun to demonstrate its value to Wales and the NHS through inward investment that has created at least 80 new jobs and the performance of national wound audits, education and training.
Among the first actions WWIC undertook was to identify both the current cost of wounds to NHS Wales and the number of hospital patients in Wales with wounds. The conservative cost of wound care in the community sector for 2013-14 in NHS Wales was calculated from Swansea University’s Secure Anonymised Information Linkage (SAIL) databases to be around £330m annually, 6% of the budget of NHS Wales.2 Extrapolating this to include secondary care costs would be in the region of 10-12% given that a chief nursing officer (CNO) commissioned audit of secondary care identified that 30% of all in-patients had a wound.3
WWIC led the national audit focused on pressure ulcers and incontinence-associated dermatitis across all hospitals on behalf of the CNO of Wales, with almost 9% of all hospital patients having pressure ulcers, 50% of these being acquired in the hospital setting, with inaccuracies in recording and categorisation of pressure ulcers also being identified.
The benefits of improved wound healing
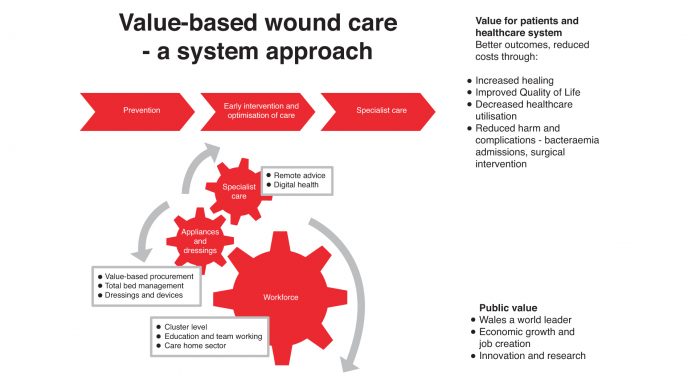
WWIC believes that a system approach to value-based wound care could have significant impact across the health economy through a focus upon three key areas – improved wound prevention, early intervention and optimisation of care, and finally access to specialist care through WWIC (Fig. 1 – above).
Understanding technology in wound healing
The role of new technologies in wound healing has increased dramatically from scenarios in the 1980s, when most wounds were left uncovered or dressed using simple gauze dressings4 to a complex environment with almost 2,000 products that can be used to help prevent and heal wounds.5 One role of a national wound centre is to provide assessment of the new and existing interventions used in wound prevention and healing.
Staff within WWIC have many years of experience around the technical and clinical evaluation of medical devices used in wound prevention and healing. Indeed, they have contributed to the development of several successful products and devices, including silastic foam and Intrasite dressings, the Repose Mattress Overlay, and the Dyna-Form® Static Air mattress.
Evaluation of wound technologies doesn’t only focus on new products; within a pilot project across four care homes in South Wales, WWIC identified that 40 of 117 mattresses (34.2%) failed visual inspection where either the mattress did not provide support to the resident or was a potential source of infection, having been soiled or stained. This finding suggests many care home residents are supplied with inadequate mattresses and highlights maintenance challenges.
A recent development has been the introduction of hybrid mattresses to the NHS. A hybrid mattress consists of a series of longitudinal air cells along the mattress that also contain foam. The hybrid mattress can be used as an ordinary mattress whereupon the patient is supported by the foam within the air cells. However, if the mattress is connected to a pump, it can be used as a more sophisticated dynamic mattress where the air cells are sequentially inflated and deflated to change the points of the body that bear weight – so better helping to prevent pressure ulcers. Significant cost savings have been reported where hybrid mattresses are used to replace traditional dynamic mattresses. Costs are saved through reducing the time required to order and supply a dynamic mattress to a ward from a reported 434 minutes to zero, as the hybrid mattress will already be on a bed and simply requires connecting to a pump unit.
In 2016 tissue viability nurses in Hywel Dda University Health Board (UHB) and Abertawe Bro Morgannwg UHB approached WWIC and the Pressure Ulcer Prevention Intervention Service (PUPIS) to help evaluate dynamic hybrid mattresses to provide a framework through which these devices could be evaluated, allowing for future procurement decisions to be made based on comparative evidence of performance. This work involved three stages – physical examination of available hybrid mattresses by tissue viability nurses, infection control, manual handling and clinical engineering, followed by WWIC and PUPIS laboratory investigation of the pressure-redistributing performance of hybrid mattresses, and, eventually, clinical evaluation of the two hybrid mattresses that excelled in the first two phases within Hywel Dda UHB.
Improving wound healing through education
Improving wound prevention and treatment is not just about the correct use of technology, as the largest proportion of the costs of wound care rests upon the time invested by a wide range of NHS staff to tackle wounds. Improving the skills and knowledge of NHS staff around wound healing is also one aspect of WWIC’s work.
A third (34.2%) of the pressure ulcers identified during the national wound audit had either not been reported by ward staff or been reported with an incorrect classification. The average cost of the treatment of a pressure ulcer varies according to the classification of its severity, with the average cost of treatment of a category I pressure ulcer (the least severe form of this wound) costing £1,214 while a category IV pressure ulcer costs, on average, £14,108.
Where a pressure ulcer is incorrectly classified (for example, a category II pressure ulcer is incorrectly described by ward staff as a category III wound) the cost of treatment will rise. The additional costs due to misclassification arise from more frequent nursing interventions and the use of more complex wound care products. The typical cost of getting the classification of a pressure ulcer wrong by a single category is £4,298. With 152 misclassified pressure ulcers seen during the single week of wound audit, the likely minimum cost of these misclassified pressure ulcers to NHS Wales was £653,296.
Where pressure ulcers were not reported by ward staff (158 pressure ulcers across the national audit) there exists the potential for delayed wound healing (and increased costs) within NHS Wales and reduced patient satisfaction with their care, while also exposing NHS Wales to potential claims for clinical negligence. This is especially true in the case of 16 patients with unreported severe pressure ulcers (category III or unstageable wounds).
WWIC has worked with GP practices in South Wales documenting the outcomes of wound treatment and associated costs before and after the introduction of standardised wound management practices and access to support from experienced clinicians within WWIC.
Prior to intervention of utilising a buddy from WWIC to work with individual practice nurses, 23 out of 57 (40.3%) wounds healed within the GP practice; post-intervention, the healing rate increased to 35 out of 54 (64.8%) – and to an impressive 85% in one practice. Costs before intervention ranged from £45 to approximately £1,375 (mean ~£250), rising slightly post-intervention to a mean of ~£316 (range £58 to £1,750). The improved healing rate and slightly higher cost were associated with the greater use of leg compression therapies post-intervention. Over time the increased cost of standardised wound treatment within GP surgeries will be offset by the reduced number of patients presenting with wounds given the increased healing rate achieved within the practice.
Learning from the first national wound centre
As the pathfinder for clinical innovation in Wales and the only body that connects NHS, academic and commercial organisations, WWIC is a catalyst that creates the right conditions to facilitate clinically effective change across the health economy as well as energising a climate for inward investment. We maximise opportunities for health and wealth creation in Wales and beyond through:
• Leading and supporting the development and adoption of wound healing innovation to include diagnostics, technologies and
care pathways;
• Driving the adoption and spread of evidence-based practice to include an MSc in Wound Healing, bespoke clinical courses, e-learning, publications and presentations; and
• Enhancing economic growth through collaboration and partnership with industry and the NHS.
Tackling the burden of wounds requires focused skills in wound prevention, early correct treatment, and the safety net provided by access to specialist care. WWIC as the first national wound centre provides these three key pillars to NHS Wales and believes the benefits already seen in Wales can also be realised by other national wound centres. WWIC looks forward to the day when it is no longer the only national wound centre worldwide as all patients deserve excellence in wound prevention and treatment.
References
1 Guest JF, Ayoub N, McIlwraith T, Uchegbu I, Gerrish A, Weidlich D, Vowden K, Vowden P. Health economic burden that wounds impose on the National Health Service in the UK. BMJ Open 2015; 5: e009283. Doi: 10.1136/bmjopen-2015-009283
2 Phillips CJ, Humphreys I, Fletcher J, Harding K, Chamberlain G, Macey S. Estimating the costs associated with the management of patients with chronic wounds using linked routine data. Int Wound J. 2015; doi: 10.1111/iwj.12443
3 Clark M, Semple MJ, Ivins N, Mahoney K, Harding K. National audit of pressure ulcers and incontinence-associated dermatitis in hospitals across Wales: a cross-sectional study. BMJ Open 2017; 7: e015616. doi: 10.1136/bmjopen-2016-015616
4 David J, Chapman RG, Chapman EG, Lockett B. An Investigation of the Current Methods used in Nursing for the Care of Patients with Established Pressure Sores. Nursing Practice Unit, Northwick Park, Middlesex, 1983
5 Mark Allen Publishing. Wound Care Handbook, accessed at http://www.woundcarehandbook.com on 28 December 2017
Professor Michael Clark, Commercial Director
Maureen Fallon, Chief Operating Officer
Professor Keith Harding, Chief Medical Officer
Welsh Wound Innovation Centre
This article will appear in issue four of Health Europa Quarterly, which will be published in February.










