Gregor Zorn of the European Cannabinoid Therapy Association (ECTA), shares his thoughts on the stigma surrounding cannabis as a medicine and the impact this has on those who need it the most.
The tide of medical cannabis acceptance is beginning to turn across Europe, yet progress is slow, and many in the medical community remain largely unaware of the benefits of the plant. Here Zorn of the ECTA explains why this is, how patients are driving change, and how the work of the ECTA is providing valuable support and education to a broad range of audiences.
Why are some doctors still reluctant to prescribe medical cannabis despite evidence of its efficacy?
Well the principal reason is the lack of education. Most doctors have never studied medical cannabis, they only know that cannabis is a drug and that it has no medical application, because that is what they were taught at the university. This poses a problem because despite the fact that this plant has been medicinally used for thousands of years, doctors are not taught anything about the history of plants with medicinal properties, nor have they studied the endocannabinoid system, the endogenous system that we all have that is the basis of how cannabis works and acts therapeutically in our bodies.
This system was discovered more than 25 years ago, and yet it is still not taught in most universities. It is a shame because it’s such an important system which brings balance – so called homeostasis to our bodies. It interacts with most of our physiological systems, so it influences all these systems, maintaining balance almost like a conductor of an orchestra if you will. It ensures that all the instruments play at the right time, in the correct tone and that everything is in harmony.
It is involved in important processes such as learning and memory, neuronal development, pain perception, digestion, inflammation, appetite regulation, energy balance, regulation of sleep, stress and emotions.
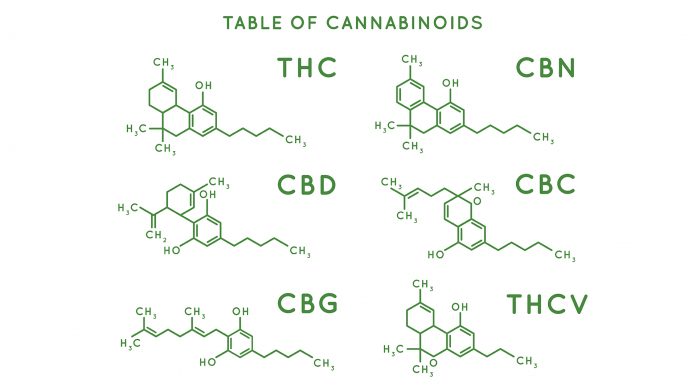
Endocannabinoids are endogenous cannabinoids that we produce and act as lipid messenger molecules. By binding to receptors present on various cells, they can modulate the molecular mechanisms of the cell, restoring balance and optimising its activity.
It is similar to the opioid system if you will. Doctors are taught about the opioid system; we have endogenous opioids and we have opioid receptors, and plant derived opioids bind to these receptors and can trigger certain effects. In the same way we have endogenous cannabinoids, which bind to the cannabinoid receptors. Plant cannabinoids can also activate these receptors, and this is the basis of how they work in our body. If the endocannabinoid system does not work correctly, due to environmental or genetic factors, disease can occur.
By taking plant cannabinoids, we can restore this imbalance and alleviate the symptoms of different types of diseases.
So, it comes back to education, there simply needs to be better teaching at the University level before doctors go on to qualify and treat patients?
Yes, absolutely. I don’t know of a doctor who comes out of university without knowing what the nervous system or the immune system are, yet many don’t know about the endocannabinoid system. This is worrying because it has so many effects on so many other physiological systems, plus it also gives us insight on how certain prescription drugs work.
The endocannabinoid system is present in all vertebrates from fish to mammals, it is even present in some invertebrates, which suggests that it has an extremely important function in all of these different species of animals.
Clearly, it is here to stay, and this is why other students, studying biology or veterinary sciences, should also be taught about the system because it is essential to understanding how we and other animals work.
How varied is the level of awareness within the medical community across the continent?
Europe is behind in a sense compared to other countries such as some States in the US, Canada and Israel, as they have had more time to implement laws and regulations on medical cannabis (MC) use. Also due to the legality issues surrounding cannabis, it has been incredibly difficult to study the plant and learn how it works because access to it was so limited. In the past, most of the funding for cannabis research went to proving the detrimental effects of this plant and its constituents. Thankfully we are now seeing an increased trend in research towards the medical applications of cannabis and really understanding how different components of this plant can help in a variety of medical conditions. It is sometimes difficult to understand how this plant with these constituents can help in so many diseases and this is one of the things also that many doctors find challenging.
In Europe the situation is very different from country to country. Currently 14 of the 28 European Union Member States have some form of medical cannabis law, but still most of them are very limited in what products doctors can prescribe, and for what conditions.
There are also issues surrounding the availability of cannabinoid-based products such as flowers, tinctures and registered prescription cannabinoids, as the preparations available also can vary widely.
This presents a further challenge for doctors, as they are unaware of what indications they can prescribe different products for. Furthermore, the recommendations for prescribing medical cannabis vary between EU countries; in some countries you can get cannabis prescribed for chronic pain while in others you can’t. The only consistency between the legislation across Europe is that cannabis is always considered the last resort when all other synthetic prescription drugs have failed, and it is never considered as the first option.
The situation in Europe is slowly progressing, mainly due to the implementation of MC regulations in economically important countries such as Germany. As there is a shortage of MC, many EU countries are seeing a great economic opportunity in filling these demands. As a consequence, they are implementing MC laws, which also benefit the patients. But the current situation is still precarious and lacking in many sectors. As an example, in countries such as Italy, that has had an MC law since 2013, they are experiencing a shortage of cannabis flowers in the pharmacies, leaving patients without their medicine. In Italy there is also the issue of insurance coverage of the costs, as it depends on the region; in some regions the insurance fully covers the costs while in others patients have to pay from their pocket.
The variation is not only from country to country, I see differences from doctor to doctor. Generally speaking, the new generation of doctors are open to cannabis and are eager to learn more about the potential of use of this plant and its constituents for their patients. Whereas the older generations, they are a little bit more sceptical and may not feel the need to learn anything new, being near to retirement. With all the legal issues surrounding cannabis and how to prescribe it, many doctors are also concerned they can get into legal troubles. They do not have these issues with prescription drugs, so why would they want to learn about this? It’s just an additional burden to them and they do not get anything from it – but the patients do.
It is the patients who are driving this medical cannabis movement in Europe as well as the rest of the world. While there are some professionals and advocacy groups doing some amazing work, it is the patients who are trying MC and seeing the benefits. They are the ones who are asking their doctors for MC prescriptions and guidance regarding its therapeutic use. Most doctors are unfamiliar with the subject and don’t know what to advise.
I’m often asked what I am doing, why aren’t you speaking to politicians and medical institutions, to try to change their attitudes towards this important issue. Ultimately it is the patients who should be doing this. They are the ones who are experiencing the benefits of MC and they are the ones who are only trying to have a normal life, without looking for financial gains. They are the voters that policy makers will have to take into account, if they are truly working for the people. Of course, it is upon us to educate all parties, to understand MC and its incredible potential therapeutic use which can improve the lives of many patients.
How is the ECTA’s work helping to improve access and educate doctors?
Well ECTA is trying to inform doctors about the basics of MC use and providing this information in the form of courses and different talks, presentations and seminars, not only for doctors, for patients and for students – for just about anybody who is willing to listen. Information is key, especially providing scientifically backed information, case studies and patient’s experiences.
This information is delivered accordingly to the background knowledge of the various groups; medical professionals, pharmacists, nurses, doctors, students, and patients. The essence of giving this information is that people understand you, being a complicated subject, you must convey this information in a way that people comprehend. When presenting to physicians, we can talk more on a technical level, while with patients you need to be more general, without complicated technical terms. Ultimately, the information we provide is scientifically backed, which is essential for gaining trust and credibility.
We also use blog posts, videos and social media to spread this information and raise the awareness of MC, which is here to stay and not going anywhere. With increasing numbers of patients using MC, if some physicians are not willing to prescribe, they should at least refer these patients to other medical professionals, who are specialised in cannabinoid therapy. This is already practiced in the medical community, where certain physicians specialise in certain diseases or certain types of therapies, and this should also be adopted in the MC space. This is something common in countries with MC laws, where we are seeing an increase in physicians specialising in cannabinoid therapy and having very good results with patients.
There are an incredible amount of studies coming out every day, about how cannabinoids work in the body, the mechanisms of action, how different types of products can be used and for what indications. It’s a very complicated area, and it is evolving all the time, we are learning literally every day new things about how to use cannabis and it is really fascinating and something that should be in at least vaguely known to medical professionals. Often patients know more than their physicians on the therapeutic potential of MC and the importance of endocannabinoid system. Many patients have reported different reactions from their physicians, when mentioning MC; many are against using it therapeutically and still regard it as an illicit drug, some just don’t know what to say, while a few are very open to it and want to learn more.
What progress has already been made with raising awareness and what challenges are there still to overcome?
It is an ongoing battle because we are not only trying to inform people, but we are trying to re-educate them. Learning new things is usually easier than relearning, as you have to use relevant scientific facts to debunk the previously learned notions that tend to stick in our brains. Besides the scientific data, listening to patient feedback is also essential. This is something that medical professionals are not so keen on, but in my opinion patients are an immense resource of knowledge and we can learn from them as much as we can teach them, as they are ones who are actually testing different MC products, different cannabinoid combinations and conveying their experiences.
Cannabis is not a one size fits all treatment– it’s difficult to try to standardise medicine for people who are not standardised. We are all individuals that react differently to medications regarding dosages, adverse events and efficacy. Even identical twins can have different reactions to the same cannabinoid preparations and other prescription drugs.
The one size fits all approach does not work with cannabis, you do need to try different products and different concentrations of cannabinoids to find the right one that can help you. This process can sometimes be fast, other times it can take months to figure out, but the results are usually extremely beneficial.
Another thing that we need to understand is that cannabis is not a panacea that treats everything; it does not work for everybody, it does not work in every indication and it does not work in every stage of the disease. Nevertheless, it does work for a lot of people and it does not have any of the serious long-term adverse events that other synthetic prescription drugs can have. This gives you the liberty of experimenting with different products and if it doesn’t work, you won’t have any serious consequences. The media often portrays THC as the bad guy, with exaggerations on its harmful effects, but in reality, there has not been a documented case of death from cannabis overdose. Not a single one in whole world. Which is something you cannot state for almost any prescription medication on the market.
It’s staggering the different hoops you must jump through if you want to access MC, compared to other legal prescription drugs. The listed adverse events for many medications can be very severe and even deadly, but the majority of patients don’t read them or give any thought to the possible implications. It does not help that some physicians disregard these adverse events as simply legal requirements that the pharmaceutical companies have to adhere to. The bias against MC is really overwhelming and you start to question why there is so much negative attitude towards this healing plant that has never killed anyone and is providing relief to millions of people.
You often hear that we need more data on MC and patients can be an extremely important source, especially if you have many patients with the same medical condition. As an example, if you have a thousand patients with multiple sclerosis using MC and 70% of them report having good results with a 1:1 THC: CBD ratio, you have a good starting point for new MS patients. While it might not work in all of them and you might have to adjust the ratio according to the patient’s feedback, it provides a good basis for beginning MC therapy.
Looking to the future what would the ECTA like to achieve?
The goal is to normalise the use of MC in healthcare in Europe and the rest of the world. Providing the possibility for patients to have this option as a viable treatment alongside other conventional treatment. This is only possible through the education of MC and through delivering scientifically backed information about the medicinal use of this plant. We have to debunk the 70 plus years of negative propaganda and re-educate the people. Patients have to know that statements that it is an addictive illegal gateway drug with no medical value, are myths which are still engraved in our brains.
Education is key and ECTA is doing this via different platforms such as educational events, as well as providing relevant information online. Educating physicians is especially important as they are the ones who will prescribe MC and providing them with understandable and scientifically backed information is key in making them more comfortable in working with these types of medications. We are also educating the patients and anyone that is interested in the subject.
It is an ongoing struggle, but I remain convinced that we are on the right side of history and we are doing this because we believe in it. After seeing numerous cases of how MC has improved, changed and even saved the lives of many patients, this is something worth fighting for.
Gregor Zorn
Director
European Cannabinoid Therapy Association (ECTA)
http://www.ect-a.com/
Please note, this article will appear in issue 10 of Health Europa Quarterly, which is available to read now.