Research cites 92 studies that assert intra-surgery feasibility of diffuse reflectance spectroscopy.
The results of the review, in which diffuse reflectance spectroscopy (DRS imaging technique) measurements from patients treated with and without neoadjuvant chemotherapy, show that contrast between healthy tissue and tumours is not altered due to neoadjuvant chemotherapy.
This suggests that the same reflectance spectral signatures can be used for tumour margin guidance independent of the chemotherapy status of the patient.
In the article published in the peer-reviewed SPIE publication Journal of Biomedical Optics (JBO), Influence of neoadjuvant chemotherapy on diffuse reflectance spectra of tissue in breast surgery specimens, the research observed across 92 ex vivo breast specimens.
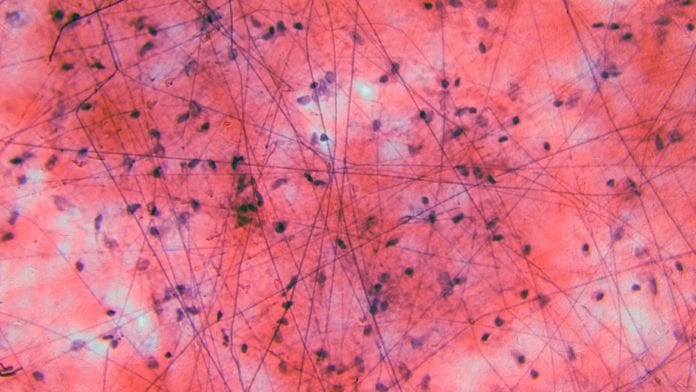
DRS imaging
Because healthy and tumour tissue can be readily discriminated, tumour-margin assessment by DRS – which can discriminate different tissue types based on optical characteristics – becomes a feasible consideration during breast-conserving surgery.
This is possible even if the patient has received neoadjuvant chemotherapy prior to surgery, a procedure that has become commonplace.
The ultimate goal of the intra-surgery application of DRS would allow the surgeon to assess the tissue while performing the resection of tumours to ensure that the resection margin is clear of tumour tissue.
According to JBO Editor-in-Chief, SPIE Fellow, and MacLean Professor of Engineering at the Thayer School of Engineering at Dartmouth College, New Hampshire, Brian W. Pogue, the paper and its findings are notable due to the large number of clinical samples analysed, and the consequent relevance to assessing neoadjuvant chemotherapy changes.
Fellow said: “While a significant amount of work has been done defining the spectral signatures of breast cancer tumours and showing that this can be used for guidance, this is one of the first attempts to examine tumours following neoadjuvant chemotherapy as well.
“The results show that the signatures do not appear to change and so the status of the patient would not confound spectral imaging to help define the lumpectomy margin.”









