Scientists based in Sweden have performed an investigation to reveal how the immune system’s natural killer cells respond to SARS-CoV-2 infection.
Research on how natural killer (NK) cells detect which cells have been infected with COVID-19 is sparse; however, an international team of scientists led by researchers at the Karolinska Institutet in Sweden have identified that natural killer cells react to a special peptide located on the surface of infected cells. The team believe that this is a potentially pivotal breakthrough in comprehending how the immune system is impacted by COVID-19.
The full findings of the study are published in Cell Reports. The Karolinska University Hospital and research laboratories and universities in Italy, Germany, Norway and the USA collaborated on the study.
What are natural killer cells?
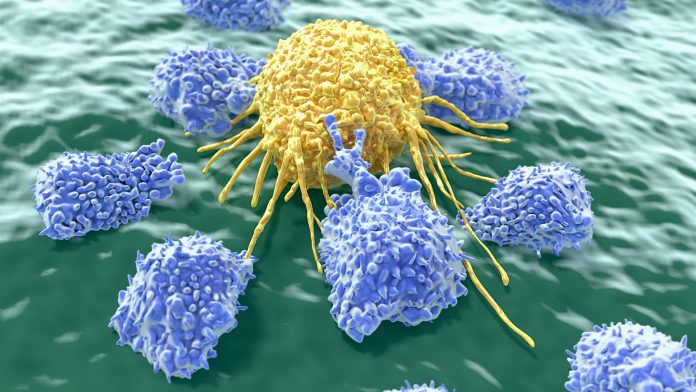
Natural killer cells are white blood cells that are part of the body’s innate immune system. However, dissimilarly to cells in the adaptive immune defence, they can expertly identify and destroy cancer cells and cells infected with viruses rapidly without having encountered them previously. This efficient process is enabled by a balance between natural killer cells’ activating and inhibiting receptors, which are proficient at reacting to various molecules on the surface of other cells.
Peptide influence
The team’s research discovered the mechanisms that allow some natural killer cells to become activated when encountering a cell infected with SARS-CoV-2. They found that infected cells contain a peptide from the virus that triggers a reaction in natural killer cells that carry a particular receptor – NKG2A – which can detect the peptide.
Quirin Hammer, a researcher at the Center for Infectious Medicine (CIM), Karolinska Institutet, said: “Our study shows that SARS-CoV-2 contains a peptide that is displayed by molecules on the cell surface. The activation of NK cells is a complex reaction, and here the peptide blocks the inhibition of the NK cells, which allows them to be activated. This new knowledge is an important piece of the puzzle in our understanding of how our immune system reacts in the presence of this viral infection.”
Initially, the team employed computer simulations to test their hypothesis, which was later confirmed in a laboratory. Then, the team infected human lung cells with SARS-CoV-2 in a controlled environment, which enabled them to identify that natural killer cells with the receptor in question are stimulated to a greater degree than natural killer cells without it.
Dr Hammer said: “These findings are important to our understanding of how immune cells recognise cells infected with SARS-CoV-2. This may become significant when monitoring new virus variants with the aim to determine how well the immune system responds to them.”
The researchers are now following up on their study with the aid of the biobank at Karolinska University Hospital and Karolinska Institutet, which has blood samples from over 300 people treated for COVID-19 during the pandemic’s first wave.
“We’ll be examining if the composition of natural killer cells a person has contributes to how severe their symptoms are when infected with SARS-CoV-2,” Hammer concluded.
The research received funding from the EU, Deutsche Forschungsgemeinschaft (DFG), the Karolinska Institutet Foundation for Virus Research, the Petrus and Augusta Hedlund Foundation, the Clas Groschinsky Memorial Foundation, the Lars Hierta Memorial Foundation, the Tornspiran Foundation, the Swedish Cancer Society, the Norwegian Research Council, the Swedish Research Council, the Knut and Alice Wallenberg Foundation and Nordstjernan AB.










