With mounting pressure on NHS services, particularly in light of the COVID-19 pandemic, Peter Harrison, Managing Director of Siemens Healthineers GB&I, outlines the benefits of community diagnostic centres as a scalable solution to diagnostic care.
The UK’s National Health Service has been under significant pressure for some time, with the need for major expansion of diagnostic capacity identified before the COVID-19 pandemic. As the impact of COVID-19 continues to unfold, the backlog of care in England sits at its greatest point in 20 years.1 Inspired by Professor Sir Mike Richards’, Diagnostics: Recovery and Renewal report, integrated care systems and hospital groups across the country are seeking to establish scalable, digitally-enabled community diagnostic centres (CDCs). These highly productive elective diagnostic centres will support the relocation of diagnostic services for cancer, cardiac, respiratory, and other conditions away from acute hospital sites – improving efficiency to help meet NHS Long Term Plan priorities.
Health system challenges
Ahead of the first cases of COVID-19 in the UK, a marked increase in breaches of the six-week diagnostic standard and outsourcing of imaging were indicators of a growing problem for the NHS.2 Demand for diagnostic services had risen rapidly over the five years preceding the Recovery and Renewal report, and new commitments from the UK government to diagnose three-quarters of cancers at an early stage by 2028 demanded reform.2,3
In comparison to other OECD countries, England lags far behind the average for diagnostic scanners per million population, and with demand for diagnostics rising faster than that for NHS services as a whole, the need for major expansion is clear.4 Significant investment in equipment is a key component of the Recovery and Renewal report which recommends a 100% expansion of CT capacity, in addition to expansion of MRI, PET-CT, X-ray, ultrasound and DEXA scanning facilities in line with pre-pandemic growth rates.5

The COVID-19 pandemic has only exacerbated existing challenges, with infection control measures and the ongoing diversion of resources lying heavily on the shoulders of the NHS. The case for change becomes increasingly urgent as the backlog of examinations generated by COVID-19 grows.
Burgeoning diagnostic demand
The long-term impact of COVID-19 on the NHS, and its patients, remains to be seen. The temporary suspension of the national bowel, breast, and cervical screening programmes, and the three million people who did not receive invites to these services, is just one example of pent-up diagnostic demand that is likely to cause capacity challenges post-pandemic.6
Although progress is being made to reduce waiting lists, the number of patients waiting more than a year for treatment is 280 times the number in June 2019.7 The Institute for Fiscal Studies has warned a significant hidden backlog of patients is yet to come forward for treatment, perhaps due to concern over COVID-19 infection or conditions that are yet to be identified. The return of just two-thirds of these ‘missing patients’ could lead waiting lists to exceed 13 million.8
Fear of visiting A&E or primary care providers is expected to have prevented patients from accessing care, evidenced by requests for diagnostics reducing during the peak of the pandemic.9 Public Health England has worked alongside the NHS to provide reassurance to both patients and staff, with the introduction of COVID-19 specific infection prevention and control (IPC) measures.
New recommendations for primary and community healthcare providers are amongst an archive of IPC guidance including recommendations for the use of personal protective equipment, social distancing, optimal hand hygiene, surface decontamination and ventilation.10 Whilst requests for diagnostics are now rising, throughput is reduced by the time taken to implement these comprehensive IPC measures.9
Fortifying diagnostic provision
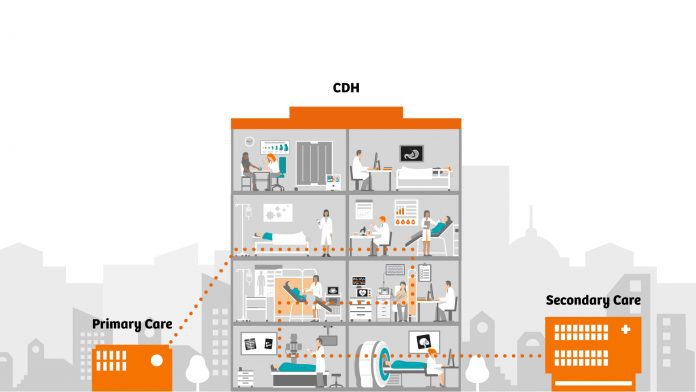
The spirit of innovation escalated by the pandemic has shown how rapidly the workforce can adapt, and there is a drive to extend this to the reformation of diagnostic provision. In the NHS-commissioned, Diagnostics: Recovery and Renewal report, Professor Sir Mike Richards details recommendations to enable the fulfilment of NHS Long Term Plan priorities. The rapid and widespread introduction of scalable, digitally-enabled community diagnostic centres is at the heart of recommendations to drive efficiency and improve service provision in the UK by supporting the division of acute and elective diagnostics.
Community diagnostic centres could tackle health inequalities and drive population health outcomes, providing quicker and more convenient access to testing, whilst improving patient experiences of the diagnostic process. The development of integrated, symptom-based pathways should be agreed upon between primary and secondary care, implementing learning from changes made as a result of COVID-19. Following the successful introduction of virtual consultations at the peak of the pandemic, many elective diagnostic tests requested by GPs or specialists could be made virtually, with tests accommodated in community diagnostic centres.
IT connectivity will form an integral part of the transformation of these services, with areas such as imaging, echocardiology and endoscopy identified as those that could benefit from enhanced digitalisation. At a granular level, this should include technological advancements such as AI to support diagnosis and the planning of care. At the broader level, this encompasses the CDC IT infrastructure at large.
COVID-19 minimal community diagnostics
At the centre of the initiative to introduce community diagnostic centres is the aim to reduce footfall at acute hospital sites. New capacity afforded by the community diagnostic centres will allow the NHS to separate elective and urgent diagnostic streams, thereby protecting elective capacity when these services come under pressure. Moving elective diagnostics into a COVID-19 minimal community setting could tackle some of the barriers to care apparent as a result of the pandemic. Patients will be able to attend screening or diagnostic appointments in locations convenient for them and with reduced risk of infection.
It has been recommended these centres should be separate from locations serving COVID-19 patients. Where co-located, separate entrances and staff should minimise transmission of the virus and appropriate cleaning and PPE regimens should be in place. Additional guidance for infection prevention should be followed, including regular testing for clinical staff, patient testing and temperature checks before appointment attendance.11
Siting these services in a COVID-19 minimal CDC can help protect service continuity for examinations deemed high-risk for COVID-19 transmission, preventing delays to diagnosis and reducing waiting times to receive these tests. At the peak of the pandemic, CT and MRI services were drastically impacted by the time taken to implement enhanced cleaning protocols between patients where the COVID-19 status was unknown. This led to reduced throughput and the number of patients waiting more than six weeks for diagnostics growing significantly following the onset of the pandemic – undoubtedly contributing to the looming backlogs the NHS faces today.2
Community diagnostic centres are not only predicted to play an important role in diagnosis but also the monitoring of long-term health conditions. Patients with this kind of condition could be asked to attend outpatient appointments for check-ups or blood tests regularly. The provision of these services in a community setting could boost attendance rates and improve experiences with one-stop offerings and more convenient access. The relocation to a COVID-19 minimal CDC would also remove the need for visits to acute hospital sites, reducing the risk of infection for patients who are more likely to be considered vulnerable to COVID-19.
Realising the vision for reform
The NHS has withstood the unprecedented challenges of a global pandemic despite fundamental issues around capacity and service provision prior to the COVID-19 crisis. The full impact of this is yet to be seen, however, there is no doubt that the pandemic will have a lasting effect. The cessation of non-COVID-19 services in the first wave, combined with drastic changes in patient behaviour, have led to a growing backlog of care predicted to take years to overcome.1

Whilst the pandemic has waiting lists at a record high, the lessons learned offer some hope.7 COVID-19 has radically changed approaches to the provision of care, with some changes previously considered impossible, achieved in weeks in the face of the crisis. Carrying this approach forward will be key to the NHS’ recovery, with the implementation of COVID-19 minimal community diagnostic centres essential to helping deliver the efficiencies required to clear the backlog of examinations and meet growing demands for diagnostic services.
Community diagnostic centres could offer countless operational benefits, creating a sustainable, efficient and digitally-enabled diagnostics service fortified to withstand the evolving pressures the NHS faces. It is essential that we embrace the learnings of the pandemic, and the opportunity for change, to ensure its legacy is one of transformation.
To discover more on community diagnostic centres, visit: www.siemens-healthineers.co.uk/CDH
References
- news.sky.com/story/covid-19-it-will-take-five-years-for-some-hospitals-to-catch-up-with-patient-backlog-experts-warn-12278863
- Diagnostics: Recovery & Renewal – p. 8
- www.supplychain.nhs.uk/news-article/nhs-england-funding-injecting-200-million-into-aged-asset-replacement/
- Diagnostics: Recovery & Renewal – p. 16
- Diagnostics: Recovery & Renewal – p. 11
- www.nature.com/articles/s41571-020-00446-0
- www.bma.org.uk/advice-and-support/nhs-delivery-and-workforce/pressures/pressure-points-in-the-nhs
- www.bbc.co.uk/news/health-58132538
- Diagnostics: Recovery & Renewal – p. 79
- www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/new-recommendations-for-primary-and-community-health-care-providers-in-england
- Diagnostics: Recovery & Renewal – p. 84
Peter Harrison
Managing Director
Siemens Healthineers GB&I
www.siemens-healthineers.co.uk/CDH
This article is from issue 19 of Health Europa Quarterly. Click here to get your free subscription today.







