Scientists at the University of Pittsburgh Swanson School of Engineering have developed a cutting-edge smart implant to monitor a patient’s progress from spinal fusion surgery.
Spinal fusion surgery is a serious procedure to treat a range of spinal conditions and involves amalgamating two vertebrae. Traditionally, a cage will be implemented to provide support where the disk once existed between the vertebrae. Now, researchers have significantly advanced this technology, designing a smart implant that acts as a cage whilst simultaneously analysing the healing process.
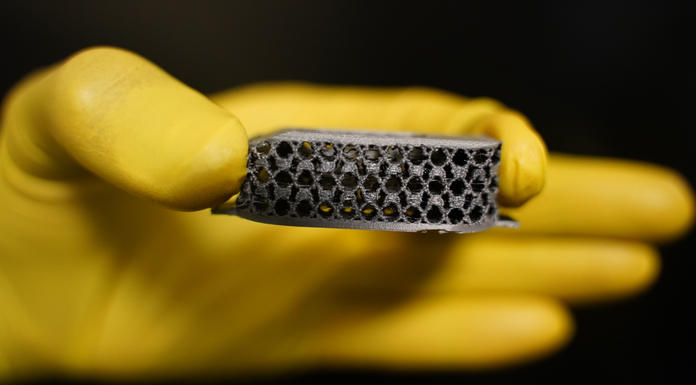
The University of Pittsburgh Swanson School of Engineering team has developed a patient-specific 3D-printed smart metamaterial implant with sensors to monitor spinal healing. The innovation has the potential to transform the future of spinal fusion surgery.
Amir Alavi, an assistant professor of civil and environmental engineering whose iSMaRT Lab led the research, commented: “Smart implants can provide real-time biofeedback and offer many therapeutic and diagnostic benefits. It is very challenging to integrate bulky circuits or power sources into the small area of implants. The solution is to use the implant matrix as an active sensing and energy harvesting medium. That’s what we’ve been focused on.”
The research is published in the journal Advanced Functional Materials.
How do the smart sensors work?
The smart sensors represent a new class of multifunctional mechanical metamaterials that act as their own sensors, recording and relaying essential information about the pressure and stresses surrounding them. The smart sensors generate their own power and can be employed for various sensing and monitoring applications.
When under pressure, contact-electrification occurs between the materials’ conductive and dielectric microlayers, emitting an electrical charge that relays information about the condition of the material matrix.
The smart sensor generates its power through a built-in triboelectric nanogenerator mechanism, removing the need for an additional power source. A tiny chip records data about the pressure on the cage, which indicates how the spinal fusion surgery healing is developing. The data is then read noninvasively on a portable ultrasound scanner. The smart sensor is also made from a highly tuneable material that can be customised for the patient.
Alavi said: “Spinal fusion cages are widely used in spinal fusion surgery, but they’re usually made of titanium or PEEK polymer materials (a semi-crystalline, high-performance engineering thermoplastic) with certain mechanical properties. The stiffness of our metamaterial interbody cages can be readily tuned. The implant can be 3D-printed based on the patient’s specific anatomy before surgery, making it a much more natural fit.”
The future of spinal fusion surgery
The researchers have already analysed the performance of the smart implant in human cadavers and are now planning to use the device on animal models. Due to being incredibly adaptive and scalable, the technology could be used for future medical applications, such as cardiovascular stents or components in hip or knee replacements.
Alavi concluded: “This is a first-of-its-kind implant that leverages advances in nanogenerators and metamaterial to build multifunctionality into the fabric of medical implants. This technological advancement will play a major part in the future of implantable devices.”









