
A growing body of research suggests that disposable wipes are a safer and more effective infection control method than reusable cleaning cloths.
From misting to spraying to fogging, customers have a wide range of cleaning tools at their disposal for delivering cleaners and disinfectants – but choosing the right delivery mechanism can be difficult. While disinfectants can simply be sprayed onto environmental surfaces to kill or inactivate pathogenic microorganisms, wiping the surface is an important part of the cleaning process and an effective way to control contamination on a hard surface. The efficacy of the disinfectant is reduced by the presence of soil particles, the removal of which is especially key. Wetting the wipe significantly enhances particle entrapment and removal in comparison with dry wiping methods. A study by Rutala (2012) in the US involving Clostridioides difficile found that two to three log of spores were removed simply through the physical act of wiping the surface with a damp cloth.
Infection control and hospital safety
A case study was conducted in the US by Parkland Health and Hospital System, in partnership with healthcare support services provider Crothall Healthcare, to develop and implement a disinfection protocol that would improve its hospital safety scores. It was important to incorporate a daily system which would be sufficiently simple for staff to consistently execute while reducing expenditures on cleaning and disinfection tools and equipment. After evaluation of Parkland’s disinfecting products and methods, Crothall implemented use of disposable Oxivir® Tb Wipes in patient rooms at the end of 2015. Incorporating the use of the sustainable hospital disinfectant has resulted in improvements in productivity, lowered costs and increased procedure compliance.
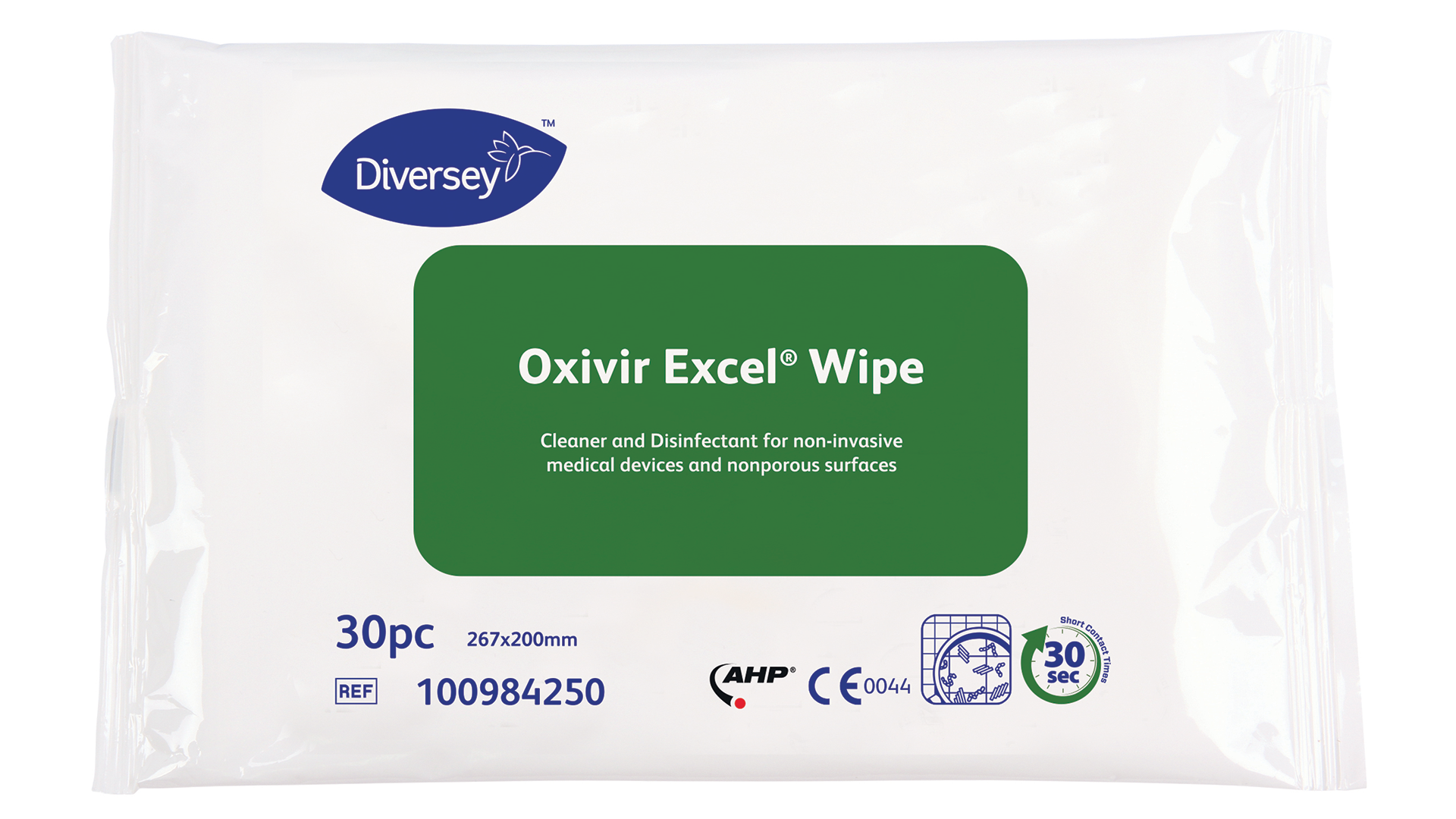
Oxivir Tb (US) and Oxivir Excel Wipes (Europe) are powered by Accelerated Hydrogen Peroxide (AHP®) technology and effective against a broad spectrum of pathogens with very short contact time (fully virucidal in 30 seconds for Oxivir Excel Wipes) important when turning over patient rooms quickly. Use of Oxivir Wipes improves compliance because surfaces remain wet for the required label contact time, ensuring disinfection while streamlining the process. The wipes are tough enough to clean and disinfect surfaces and equipment, while being gentle on staff, equipment and surfaces.
Since the implementation of a new programme which encompasses products, processes and procedures, Parkland has seen impressive results including cleaning time decreased by 12 minutes for discharges and 20% for daily cleaning. ATP testing showed improvement on high-touch cleaning by approximately 50%.
According to Crothall Healthcare General Manager Alan Williams, the disposable disinfection wipes have improved both cleaning performance and Parkland’s bottom line. “Utilising Oxivir Tb disposable wipes has eliminated my daily headaches managing the laundry process,” Williams said. “We no longer have to manage the laundering procedures for the microfibres and rags, and employees have the tools they need to do their jobs every day.”
Eliminating this pain point and expense has allowed Parkland management to focus on its most important job: that of reducing the incidence of healthcare-associated infections (HAIs). Williams reports that expenditure ranged between €800 and €1600 on replacement cloths each week. It is now easy for Parkland staff to perform their jobs in less time because they no longer have to return to the cart to get new rags or dip their rags in disinfectant. According to Williams, switching to Oxivir Tb Wipes was a game changer for dwell time alone, because the AHP-powered wipes are not corrosive and surfaces remain wet without double wiping.
Improving the user experience
Another case study was performed at Saint Luke’s Health System Quality Department and Saint Luke’s Hospital (SLH), in Kansas City. The team identified the opportunity to improve the hospital’s quality, implementation and outcome of products and procedures which directly impact its scores. The Saint Luke’s Health System Green Team was included in the review and decision process with the purpose of identifying products and processes to customise and improve across the entire hospital organisation.
“Members of the Infection Prevention team, Nursing Council, and the Green Team noted that the accelerated hydrogen peroxide in the Oxivir wipes was a better cleaner than they were using before,” said Amir Jahansouz, Director of Environmental Services at Crothall Healthcare. “The convenience of a pre-moistened wipe was another important factor in the decision because it ensures the product is always diluted correctly and the wipes are clean and fresh with each use, important in discouraging transmission of pathogens through the rags.”
The rise of disposable wipes
A recent study, published in the Infection Control and Hospital Epidemiology journal by Dr Timothy Wiemken and colleagues at the University of Louisville, evaluated the value of using ready-to-use (RTU) wipes. When compared to the traditional towel and bucket method, RTU wipes significantly increased compliance by 35%, decreased time to clean patient rooms by 23%, and reduced cost by €31.70 per employee per day.
The authors concluded that the increased compliance with cleaning and disinfection practices may be due to the ease of use of these products, including the convenience of obtaining new wipes when they become dry or contaminated. This, in turn, reduces the personnel time required. It is well-known that compliance with cleaning and disinfection practices in acute care patient rooms, operating rooms, and outpatient clinics is suboptimal which may contribute to an increased risk of pathogen transmission. The significant increase in compliance when using the RTU wipes may contribute to a decrease in healthcare-associated infections, which in itself may offset the cost of RTU wipes. Switching to RTU wipes may help healthcare facilities improve patient and employee satisfaction by eliminating the less effective towel and bucket method. The era of the cloth towel is gone, just like the old-fashioned handkerchief, as single-use tissues have become the standard and hygienically acceptable method to blow the nose. Towels and buckets are less hygienic, more costly, and less compliant and should be replaced by RTU.
Cleaning cloth contamination
A recent study from Arizona, conducted by the microbiologist Chuck Gerba, showed that laundered cleaning cloths are routinely contaminated with bacteria. 93% of sampled cloths (28 out of 30) from 10 different hospitals contained viable bacteria after laundering (three cloths were collected per hospital, with eight hospitals using cotton and two using microfibre cloths). The average bacterial load was 133CFU/cm2. Species identified included Pseudomonas, Klebsiella and Aspergillus fungi. The microfibre towels had higher numbers of bacteria present than the cotton cloths.
Overall, employees are comfortable using the wipes when patients are present; and by observing the housekeeping staff cleaning with the disinfectant wipes, patients are left with a positive impression which is then reflected on their satisfaction scores. The use of pre-moistened wipes offers additional benefits in terms of improved productivity, reduced validation, increased process control and repeatability, improved safety and contaminant reduction.
In summary, pre-moistened disinfectant wipes can improve hygiene outcomes by providing mechanical action in wiping surfaces and reducing the complexity of the cleaning process by eliminating the challenges associated with managing used cleaning cloths, including cost, inadequate laundering, and storage requirements.
References
- Wiemken, TL et al. The value of ready-to-use disinfectant wipes: Compliance, employee time, and costs. Am J of Infect Cont, Volume 42, Issue 3, March 2014, Pages 329–330
- Sifuentes, LY, Gerba, CP, et al. Microbial contamination of hospital reusable cleaning towels. Am J of Infect Cont, 2013; 41: 912-915.
- Rutala, WA, Gergen, MF, Weber, DJ. Efficacy of different cleaning and disinfection methods against Clostridium difficile spores: importance of physical removal versus sporicidal inactivation. Infect Control Hosp Epidemiol. 2012; 33: 1255–8.
- West, AM, Teska, PJ, Oliver, HF. There is no additional bactericidal efficacy of EPA registered disinfectant towelettes post-surface drying or beyond label contact time. Am J Infect Control. 2018; 7: 122.2018.07.005.
This article is from issue 16 of Health Europa. Click here to get your free subscription today











