icometrix is committed to democratising the personalised management of multiple sclerosis through digital health innovation
Research in multiple sclerosis (MS) treatments has brought tremendous progress. Since the launch of the first drug in 1993, the health of MS patients, expressed in quality-adjusted life years (QALYs), has increased by 66% thanks to the availability of more than a dozen disease-modifying drugs. The development of drugs for MS therapies remains a rapidly evolving market. Despite these efforts, one out of four patients currently begins their therapy in receipt of a suboptimal treatment, all while the price of new and existing disease-modifying treatments keeps rising.
Wouldn’t it be a better investment to get every patient on the best possible treatment from the start? This is where personalised medicine plays a valuable role. Identifying the optimal MS therapy for a patient from the start can improve their health by up to 34%: the equivalent of half of the pharmacological progress made over the last 30 years.
Today, disease-modifying therapies (DMTs) aim to slow down relapses and clinical disease progression. What lies ‘below the surface’ (subclinical) is just as important as what we see ‘above the surface’ (clinical). Subclinical progression is identified by lesions and atrophy in the brain and spinal cord. These biomarkers are becoming increasingly important as a therapeutic target, as they have been shown to be predictive of irreversible clinical damage.1 Recent recommendations for the use of DMTs in treating MS suggest initiating therapy sooner in newly diagnosed patients and administering high-efficacy medication to patients with very active forms of the disease. In addition, a treatment switch is advised in cases of persisting disease activity. (1,2) The choice of therapy and the need for a treatment switch both depend heavily on the level of disease activity. Personalised medicine offers the potential to optimise treatment decisions and increase the impact of treatments by more than 50%, by assessing both disease activity (clinical and subclinical) and the risk of side effects. (3)
The need for remote patient monitoring
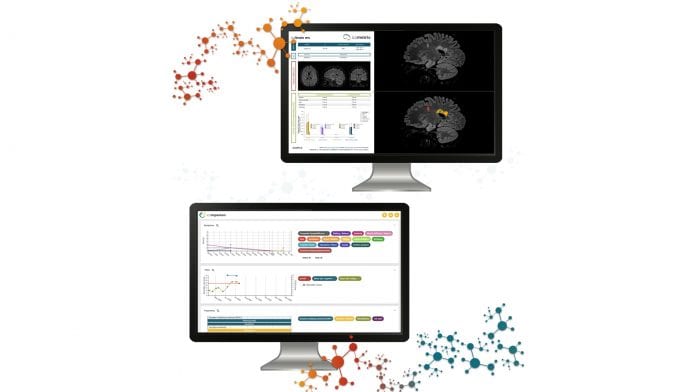
Despite the significant role of managing and reducing relapses in the care of MS patients, many go unreported. According to a survey in the UK, one in two people with MS fail to report a relapse, (4) highlighting the importance of close monitoring. A patient’s wellbeing, relapses and symptoms are reviewed during their annual neurology consultation, but due to the long period of time between neurological visits, patients often fail to recall more distant events, resulting in a biased and limited reporting of symptoms. Remote patient monitoring tools such as icompanion make way for more continuous and objective monitoring, by allowing patients to log symptoms in a standardised format on a day-to-day basis. Visualising these health statistics, together with treatment overviews and custom pre-consultation questionnaires in the centralised icompanion dashboard, allows MS care teams to be more efficient and better informed.
Evolving treatment guidelines
Guidelines across the globe – including the McDonald criteria, the American Academy of Neurology (AAN), and Brain Health Recommendations – highlight the importance of magnetic resonance imaging (MRI) in both the diagnosis and follow-up of MS. To assess treatment responses, different scoring systems have been developed, most of which take into account relapses and the emergence of new and growing lesions. (5)
With the emergence of more efficacious DMTs, a ‘no evidence of disease activity’ (NEDA) approach becomes more realistic. The NEDA concept initially identified suboptimal treatments by the presence of relapses, worsening of disability, or lesion change. However, in recent years it has become clear that brain atrophy is also an important biomarker, as high-efficacy DMTs are able to normalise the accelerated brain volume loss in MS patients. (6) ‘Silent’ progression of MS caused by brain atrophy is a major contributing factor of long-term disability in patients without relapses, suggesting that the underlying process of secondary progressive MS likely begins far earlier than is generally recognised. (7)
The relevance of brain atrophy in treatment monitoring is reflected in recent guidelines and recommendations from the Magnetic Resonance Imaging in Multiple Sclerosis (MAGNIMS) research group and the Consortium of Multiple Sclerosis Centres (CMSC), as well as scoring systems such as Rio-4 and NEDA-4; and range from qualitative assessment to quantitative cutoffs. The inclusion of brain volume changes increases the sensitivity to predict treatment responses and can result in a threefold higher probability in detecting treatment failure, thus, reducing the average time a patient is on suboptimal treatment from 3.9 to 1.3 years. (8,9)
The need for software-assisted MRI monitoring
Lesion change tracking in a clinical setting is tedious and is highly dependent on the experience and specialisation of radiologists. This prompted the introduction of assistive software in clinical practice to align, segment, and colour coded MRI scans, increasing the radiologist’s sensitivity up to 300%. (10,11)
The introduction of brain atrophy assessment, initially qualitatively but recently also quantitatively, into treatment guidelines has made the inclusion of software-assisted brain volume loss computation such as icobrain essential. icobrain, a CE-marked and FDA-cleared medical device software, leverages Artificial Intelligence to quantify MRI scans and benchmark data in an automated and standardised way to make data-driven insights possible for clinicians. Through quantitative measurements, icobrain helps to confidently incorporate lesion changes and brain atrophy into the clinical reporting and decision-making for MS patients.
Digital health in multiple sclerosis care
Treatment management in MS evolves with technology, while simultaneously giving rise to technological innovations. By leveraging digitalisation and Artificial Intelligence, barriers to integrated and personalised care can be overcome. Digital health solutions such as icompanion and icobrain connect radiologists, neurologists, MS care teams, and MS patients in an integrated and constructive way. By delivering a holistic solution to multiple stakeholders throughout the MS care continuum, providers can accomplish a significant clinical and health economic impact in the management of the second most costly chronic condition.
icompanion and icobrain allow physicians to make disease progression measurable and actionable, leading to more informed and evidence-based treatment decisions. Through this, icometrix contributes to the democratisation of personalised care for people with MS, providing individual patients with the right treatment at the right time.
References
1) Giovannoni, G., et al. (2015). Brain health: time matters in multiple sclerosis. https://doi.org/10.21305/msbh.001
2) Costello K, et al. (2019). The use of disease-modifying therapies in multiple sclerosis: principles and current evidence. A consensus paper by the Multiple Sclerosis Coalition.
3) Hult, K. (2017). Measuring the Potential Health Impact of Personalised Medicine: Evidence from MS Treatments. https://doi.org/10.3386/w23900
4) Duddy M, et al. The UK patient experience of relapse in Multiple Sclerosis treated with first disease modifying therapies. Mult Scler Relat Disord. 2014 Jul;3(4):450-6.
5) Trojano M, et al. (2017). Treatment decisions in multiple sclerosis – insights from real-world observational studies. Nat Rev Neurol. 13(2):105-118.
6) Ontaneda, D, et al. (2020). Determining the effectiveness of early intensive versus escalation approaches for the treatment of relapsing-remitting multiple sclerosis: The DELIVER-MS study protocol. Contemporary Clinical Trials, 95, 106009.
7) University of California, San Francisco MS-EPIC Team, Cree, et al. (2019). Silent progression in disease activity-free relapsing multiple sclerosis. Annals of Neurology 85(5), 653–666.
8) Sá, MJ, et al. (2014). Relapsing-remitting multiple sclerosis: patterns of response to disease-modifying therapies and associated factors: a national survey. Neurology and therapy, 3(2), 89–99.
9) Río J, et al. (2012). Change in the clinical activity of multiple sclerosis after treatment switch for suboptimal response. Eur J Neurol. 19(6):899-904.
10) Dahan, A, et al. (2018). Computer-Aided Detection Can Bridge the Skill Gap in Multiple Sclerosis Monitoring. Journal of the American College of Radiology: JACR, 15(1 Pt A), 93–96.
11) van Heerden, J, et al. (2015). Improving Multiple Sclerosis Plaque Detection Using a Semiautomated Assistive Approach. AJNR. American Journal of Neuroradiology, 36(8), 1465–1471
Wim Van Hecke PhD
CEO
icometrix
+32 16 369 000
info@icometrix.com
www.icometrix.com
www.icompanion.ms
This article is from issue 16 of Health Europa. Click here to get your free subscription today.







