
Could the NHS be driving surplus demand and by extension additional strain on services such as emergency care?
The pressures of patient demand on emergency care services continue to be reported in England evidenced by declining performance of emergency departments (EDs) against the national four hour standard1 and increased crowding,2 evidenced by higher numbers of 12 hour trolley waits and diversions of ambulances.3,4
The ambulance service is also under considerable pressure with the number of calls doubling in the last ten years (over 9 million per annum).5 The NHS Long Term Plan6 has announced some key areas for addressing the challenges faced by urgent and emergency care systems.
There is a focus on reducing pressure on emergency services in a hospital setting through:
- The development of urgent treatment centres and the introduction of same day emergency care aimed at reducing attendances at EDs and unnecessary hospital admissions;
- providing better care for care home patients, better support for palliative patients and patients with mental health conditions leading to reductions in avoidable attendances and admissions; and
- opportunities for using advanced triage techniques, decision support and redirection to other sources of care within the ambulance service alongside the use of expanded workforce models to plug existing gaps.
However, there is scant focus on how these changes will be delivered by an already overstretched workforce in order to address the anticipated reduction in demand. It is clear that there are huge opportunities for delivering technological and data driven solutions to these challenges including advanced triage techniques for patients ensuring the most cost effective and safe use of services, on scene decision support for expanded workforces and early identification of potentially avoidable hospital admissions (Fig. 1).

Studying the living eco-system
The Yorkshire and Humber (Y&H) region, includes 13 acute hospital trusts with 19 type 1 EDs (which see all types of patients and provide the full range of services – type 1 EDs encompass around 10% of the total in England) which range in size from major trauma centres to smaller rural departments served by a single ambulance provider. The region has a population of 5.5 million representing a mixture of large urban, smaller urban, suburban and rural settings and as such is a highly representative region of the UK (Fig. 2).

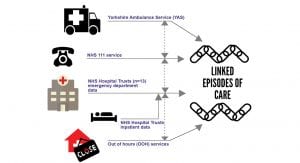
Routine NHS data from these providers of urgent and emergency care (UEC) has been linked together to provide a coherent picture of demand within Yorkshire and the Humber. Individual provider data exists, such as ambulance, 999 and emergency departments, but there has been no attempt to link data together to demonstrate patient flow across the whole system, in order to understand how it is used from the point of contact (such as a call to 999 or NHS 111) through different parts of the system (into ED and into hospital) (Fig. 3).
Linkage has now been achieved for around 15 million episodes of care within this system. This dataset is unique and provides an insight into how patients are using the system and what their outcomes are within it. This article reviews some of the findings from analysis of the data in the dataset.
Avoidable attendances at the emergency department
It has been reported for some time that a proportion of attendances to EDs are amenable to management in settings providing a lower level of care such as primary care, walk in centres and urgent care centres.7,8 These attendances (variously described as nonurgent, avoidable or inappropriate)9 are an indicator of emergency and urgent care systems which could perform better, particularly if such attendances are conveyed by ambulance.8,10
In part due to the differences in definitions, the precise size and nature of the problem of avoidable attendances remains unclear, with some estimates ranging from four to 40%.9,11
However, essentially these patients are those not requiring the full range of facilities offered by a typical consultant led emergency department in order to manage their healthcare problem. We have used validated techniques to define avoidable as identifying ‘first attendance with some recorded treatments or investigations all of which may have reasonably been provided in a nonemergency care setting, followed by discharge home or to GP care.’
Through applying this algorithmic approach to our dataset, we have been able to identify the proportion of children and adult patients who attend our region’s EDs avoidably. We have described who these patients are in Box. 1. The data shows high numbers of patients accessing the ED for themselves or their children with problems that are of very low acuity. These are often younger adults attending in the out of hours period.
Box. 1:
Feature of patients attending the emergency department avoidably
- 7% of all children attending ED (range: 13.6 to 37.7%);
- 23% of all adults attending ED (range 14.9 to 30.6%);
- Adults attending avoidably are significantly more likely to be younger (59% under 44 years);
- 20% of adults arrive by ambulance have an avoidable attendance; and
- 62% of adults attend ED during the out of hours periods with an avoidable presentation.
NHS 111 journeys
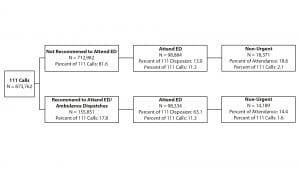
The project was the first to link data from the NHS 111 telephone advice service to subsequent ED attendance. As such we have demonstrated the proportion of patients told to attend the ED by NHS 111 who actually do, and conversely, those told not to who also subsequently attend. From this we have calculated the proportion of those attendances that were avoidable (Fig. 4).
The data demonstrates that the majority of callers to NHS 111 are advised not to attend the ED or have an ambulance response (81.6%) – this reflects the very low acuity nature of the calls overall. However, 22% of all ED attendances call NHS 111 first and of these, half are told not to go to ED (but still do anyway). When looking at avoidable ED attendances, we find that 20% of all avoidable attendances had contact with NHS 111 beforehand.
These findings indicate that there could be problems with the algorithms being used by NHS 111 – either over-triaging patients to services that they do not require or directing patients to services that are not available at a time when they are needed – thus defaulting to an ED visit.
Ambulance journeys
When we examined ambulance journeys across Yorkshire and the Humber we found that from a total of 404,458 ambulance conveyances there were 65,360 patients who accessed the ED via ambulance with a low acuity problem (16.2% of all ambulance conveyances). Higher numbers of these avoidable cases were in the out of hours period (1:5).
Amongst 16-35 year olds this rose to 1:3 cases being conveyed avoidably to the ED. Analysis of the diagnoses for these patients identified the ‘big five’ potentially avoidable conditions; minor illness, alcohol intoxication, head injuries, mental health conditions and chest pain. Additional decision support for paramedics could reduce the number of avoidable ambulance conveyances. Data science protocols could be applied to datasets such as ours to deliver solutions leading to reducing avoidable waste within the urgent and emergency care system.
Four hour target performance
For over 15 years now England’s emergency departments have been subject to a four hour target. This means 95% of all patients attending the ED need to be seen, treated and discharged within a four hour window. The target was introduced to try and improve flow in an ED and wider hospital and to reduce the number of patients waiting for long periods on hospital trolleys in corridors.
In Fig.5, we divided our patients into those who were nonurgent (or attendance was avoidable), urgent but not admitted to hospital and urgent and admitted to hospital. Plots of our data demonstrates how the four hour target performs in relation to acuity of patients presenting to the ED. The red line denotes four hours. As can be seen there is a pattern for all patients whereby the majority of patients are seen well within the four hour timeframe. However, there is a spike of activity just before the four hour point and a tail afterwards for those patients who breach the target.
The plots clearly show that the least ill (non-urgent) benefit the most from the four hour target, being seen and discharged well within the four hour window. Even those patients subsequently seen as urgent but discharged, are seen and discharged promptly. We found that admitted patients are most likely to leave in the last 20 minutes and also to breach the four hour time point. They are also likely to be older and the sickest patients in the department.
These distributions clearly demonstrate that flow into the hospital is still a significant problem. It also demonstrates that there have been unintended consequences with the introduction of the target. These include benefits for the younger and healthier patients, and the ability to ‘game’ against the target as the ‘spike’ occurring before the four hour time point shows, where patients appear to be ‘moved’ at the last minute.
Summary
Our dataset has proved extremely valuable in understanding which patients are using the urgent and emergency care system, how they are using it and what happens to them following an interaction within this system.
It is clear that there are high levels of demand within the system. However, some of that demand appears to be being driven up by the system itself. The proportion of patients attending the ED avoidably is high – leading to additional, but avoidable burden on the system. Many patients are accessing the ED with primary care problems either because they cannot access their own GP, or because they want the convenience of an ED – with no appointment needed, attending an out of hours one stop shop with short turnaround times.
Whilst access to primary care is clearly a huge problem which inevitably is driving up demand for EDs, the existence of a target that we have clearly shown benefits the least ill must also be a factor in this. We found the median turnaround time for patients attending EDs avoidably was 90 minutes – this is without any appointment, at a time convenient to the patient. This drives up brand awareness, satisfaction and therefore demand.
Similarly, we found that other services are driving some of the demand – NHS 111 and 999 services are sending patients to EDs who have very low acuity problems. The costs of this are significant alongside the resource requirements to deliver it.
Solutions should focus on the early identification of patients who can be directed elsewhere. Advanced machine learning techniques could support decision making and disposition of patients to either self care with reassurance or alternative pathways of care; thus curtailing their time within the system, but also reducing demand on those front end services. Current triage systems are poor and outdated at doing this accurately.
Working with industry partners would speed up the delivery of these solutions. Secondly, introducing parity across the system in terms of access to care. It is illogical that patients must navigate the primary care system to get an appointment, when they can turn up at their ED when it is convenient to them and get a similar level of care. Methods for developing a single point of access for all patients into urgent care alongside advanced triage techniques would begin to produce some element of control, leading to a managed system where resources can be planned and distributed effectively and patients managed safely.

References
- Monitor. A&E Delays: why did patients wait longer last winter? London: Monitor; September 2015.
- Blunt I. Quality Watch. Focus on: A&E attendances: Why are people waiting longer? London: A joint report from The Health Foundation and Nuffield Trust;2014.
- Boyle A, Higginson I, Smith S, Henderson K. Crowding in the Emergency Department. 3rd ed: College of Emergency Medicine; 2014.
- Appleby J and Dayan M. Nuffield Winter Insight: Briefing 3, The Ambulance Service. Nuffield Trust, April 2017.
- Health and Social Care Information Centre (HSCIC), Ambulance Services 2014-15. June 2015. http://www.hscic.gov.uk/ catalogue/PUB17722/ambu-serv-eng-2014-2015-rep.pdf]
- NHS England https://www.longtermplan.nhs.uk/. June 2019
- Lowy A, Kohler B, Nicholl J. Attendance at accident and emergency departments: Avoidable or inappropriate? J Pub Health Med 1994;16:134-140.
- Dale J, Green J, Reid F, Glucksman E. Primary care in the accident and emergency department: I. Prospective identification of patients. BMJ 1995;311(7002):423-6.
- Carret ML, Fassa AC, Domingues MR. Inappropriate use of emergency services: a systematic review of prevalence and associated factors. Cad Saude Publica. 2009;25(1):7-28.
- 10 MCRU Report Nicholl J, Coleman P, Jenkins J, et al. The emergency and urgent care system. Final report to Department of Health 2006–2010. Sheffield: Medical Care Research Unit.
- 11 Bickerton J, Davies J, Davies H, Proctor S, Apau D. Streaming primary urgent care: a prospective approach. Primary Health Care Research Dev 2012:13;142-152.
Professor Suzanne Mason
CURE group
The University of Sheffield
+44 (0)114 2220694
s.mason@sheffield.ac.uk
Tweet @profsuemason
Please note, this article appeared in issue 11 of Health Europa Quarterly, which is available to read now.








