Researchers from the University of Helsinki and Stanford University investigated whether transcranial magnetic stimulation (TMS) could transform the way depression is treated, especially in patients who do not respond to more traditional methods such as medication.
“Magnetic stimulation is an effective treatment for patients whose depression is not alleviated by medication. However, about half of these patients do not receive significant help from TMS. The biomarker we studied may help predict who will benefit from the therapy. In the future, it may also be possible to tailor the treatment individually,” commented postdoctoral researcher Juha Gogulski from Stanford, University of Helsinki and Aalto University.
What is transcranial magnetic stimulation?
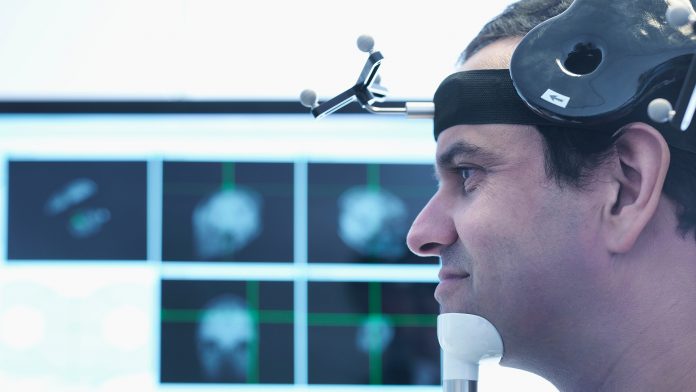
Transcranial magnetic stimulation (TMS) is a non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain.
It works by placing a magnetic coil against the patient’s scalp, and it generates brief magnetic pulses which pass through the skull and induce small electrical currents in the brain. These electrical currents stimulate nerve cells in the targeted brain region.
It is primarily used for major depression disorder (MDD), but there is ongoing research on the effectiveness of TMS for conditions such as anxiety and Parkinson’s disease.
The research team analysed which factors in targeting transcranial magnetic stimulation influence the brain’s electrical responses. They examined the behaviour of a specific electrophysiological marker. This marker could potentially be used as a biomarker in the future to measure the efficacy of TMS treatment and thus help target and tailor the therapy.
Personalised treatment is important
The first study addressed an electrophysiological marker that describes cortical excitability and the sources of error affecting its measurement. The researchers studied healthy subjects to determine how magnetic stimulation targeted the prefrontal cortex and the angle of the stimulation coil affected cortical excitability, that is, the responses measured on an electroencephalogram (EEG) immediately after the stimulation pulse.
“The results showed that targeting the stimulation coil in different parts of the prefrontal cortex significantly affected the quality of electrical responses. Additionally, we found indications that individual optimisation of the stimulation site and coil angle may further improve the quality of this metric,” said Gogulski.
The second study looked at the reliability of the same electrophysiological marker in the prefrontal cortex. The study revealed that the most significant factor affecting reliability was the stimulation site.
“Before we can develop personalised TMS therapy, we must ensure that the excitability of the prefrontal cortex can be measured as accurately as possible in individual patients to be able to monitor how TMS treatment changes brain excitability. Determining reliability is also essential before this type of biomarker can be applied clinically,” commented Gogulski.
More research is essential
Currently, transcranial magnetic stimulation does help select patients, but the effectiveness of this therapy varies between individuals. More personalised treatment could improve outcomes.
“There are many possible factors in TMS therapy that could be used for individual tailoring, such as the stimulation site, the number and frequency of pulses, the intensity of the stimulation, and the number of treatment sessions. The side effects of TMS therapy are minimal, with the most common being a temporary, mild headache.”
According to the researchers, the new studies are significant as a detailed systematic mapping of the electrical responses of the prefrontal cortex, and their effectiveness has not been done before. The team hopes that in the future, the efficacy of transcranial magnetic stimulation can be monitored by measuring the brain’s electrical responses during treatment. Based on these measurements, it might be possible to fine-tune the stimulation if necessary, even during the treatment.
“The results of both studies will be utilised in the future when designing individual brain stimulation therapies based on electrical biomarkers. However, more research is needed before new treatment methods can be implemented,” said Gogulski.









