Cancerous cells in an aggressive type of childhood brain tumour have been discovered working together to infiltrate the brain, which could lead to much-needed new treatments.
Published in Nature Medicine and funded by Cancer Research UK, the study investigated a type of childhood brain tumour called diffuse intrinsic pontine glioma (DIPG), shining a light on its most aggressive characteristic of being able to leave the brain stem and send cancer cells to invade the rest of the brain.
DIPG is a very hard disease to treat, with all children who have this type of cancer ending up dying within just two years.
What did researchers find out about DIPG?
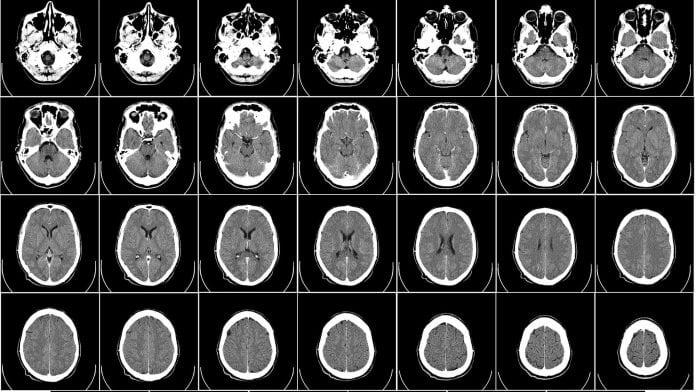
The researchers, led by a team at The Institute of Cancer Research, London, UK, used donations of biopsy tissue and the brains of children who had died from DIPG to look deep into the tumour and learn more about its cells.
It was found that DIPGs are heterogenous, which means they are made up of more than one type of cell. This enables the cells to co-operate to leave the original tumour and travel into the brain. Scientists say this shows how complex the genetic make-up of the disease is and that a multi-pronged attack is likely to be necessary for treatment.
Professor Chris Jones, who led the study at The Institute of Cancer Research, London, said: “This is the first time we’ve observed this sort of interaction between different tumour cells in DIPG. The idea that the cells are working together to make the disease grow and become aggressive is new and surprising. Childhood cancers were thought to be very simple, but this shows us that isn’t always the case. Crucially, this gives us hope that we can develop new treatments.”
He added: “Children usually can’t have surgery, because of the tumour’s location in the brain stem which controls functions such as breathing, heart rate, blood pressure, and swallowing. And other treatment options such as chemotherapy don’t work, because it’s relatively difficult to get drugs into the brain stem and many DIPG tumours have an inbuilt resistance to chemotherapy.”
In this study, researchers saw one type of cell leaving the original DIPG tumour site and migrating into the rest of the brain. This happens early in the evolution of the disease and is a cell type found in relatively small numbers.
What’s the next stage of childhood brain tumour research?
The next stage will see researchers looking for treatments that target the most important subpopulations of cells in the tumour and/or interfere with the co-operation between cells.
Professor Richard Gilbertson, director of the Cancer Research UK Cambridge Centre at the University of Cambridge, added: “This research begins to unravel the complex community of cells that make up DIPG. Through an elegant combination of molecular and cell biology techniques, this study provides a window into the heart of these tumours, allowing us to begin to decipher how their different cell populations interact with each other to promote the disease. It is exactly this sort of research that is needed if we are to beat this devastating cancer.
“Cancer Research UK recognises more must be done to tackle this devastating disease and has committed £25m [~€28m] to brain tumour research over the next five years. Brain tumours have been identified as a cancer of unmet need; survival rates have not changed significantly in a generation.”









