Presented at the Annual European Congress of Rheumatology, study supports bisphosphonate use prior to denosumab to prevent loss of bone mineral density in post-menopausal women.
Significantly more patients with stable bone mineral density after discontinuation of denosumab received zoledronate prior to initiation of denosumab, and the results of a study presented found the risk of bone mineral density loss after denosumab discontinuation is associated with younger age, high bone turnover markers, and not receiving the bisphosphonate, zoledronate, prior to initiation of denosumab – looking specifically at post-menopausal women.
Details of the study
The study followed 71 post-menopausal women who were classified into ‘loser’ or ‘stable’ groups based on their bone mineral density loss one year after discontinuation of denosumab.
Between group analysis revealed that, at initiation of denosumab, the ‘loser’ group was significantly younger, with higher level of the bone turnover marker. The use of bisphosphonates after denosumab discontinuation was comparable between groups; however, interestingly none of the ‘loser’ group had received zoledronate prior to initiation of denosumab vs. 12% of the ‘stable’ group. Other pre-denosumab characteristics were not different.
“Our study suggests that being younger, having higher bone turnover markers and not having received zoledronate before denosumab introduction increase the risk of bone mineral density loss following discontinuation of denosumab,” said Dr Bérengère Aubry-Rozier, Rheumatology Unit, Lausanne University Hospital, Switzerland.
“Our results support the use of denosumab after a bisphosphonate to reduce the bone mineral density loss at its discontinuation, and close monitoring of sCTX to maintain levels below the upper limit of the normal range for pre menopausal women.”
What do you know about Denosumab and Bisphosphonates?
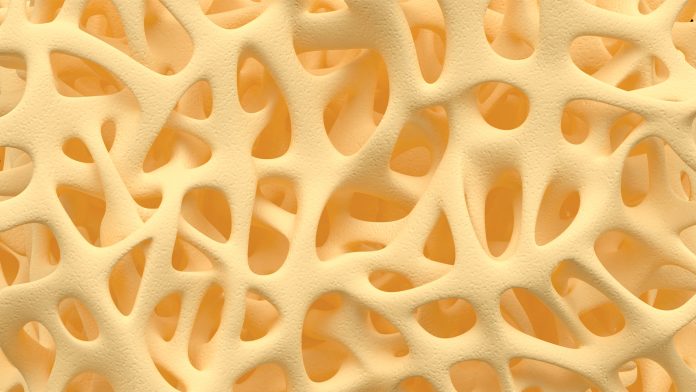
Denosumab is a human monoclonal antibody that prevents the maturation of osteoclasts by binding to and inhibiting NF-κB ligand (RANKL), a central regulator of bone metabolism.
Bisphosphonates, such as zoledronate, act mainly by inhibiting osteoclast-mediated bone resorption and are characterised by their high affinity with bone and a long half-life within the skeleton.
This long-lasting retention on bone provides a residual treatment effect on bone resorption even after treatment discontinuation. In contrast, the effect of denosumab is limited to the period of drug exposure. Moreover, the discontinuation of denosumab is associated with significant bone turnover rebound, rapid loss of bone mass, and a risk of multiple vertebral fractures.
1%-10% of patients are at risk of multiple vertebral fractures, with a median of five vertebral fractures in the seven to 20 months following denosumab discontinuation.
“There has previously been a lack of evidence related to the risk of fracture following discontinuation of denosumab and measures to prevent it,” said Professor Hans Bijlsma, President, EULAR.
“Therefore, we welcome these data that will contribute to our understanding in this area.”










