The world’s first scientific acoustic instrument that renders sound visible in water – the CymaScope – may help surgeons differentiate between healthy and cancerous cells during surgery.
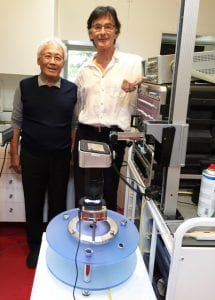
When conducting surgery to remove cancerous tumours, it can be difficult for surgeons to differentiate between healthy and cancerous tissues at the margin of a tumour. The CymaScope instrument, developed by acoustic-physics researcher, John Stuart Reid, is now being used to tackle this challenge, which could, in future, increase positive clinical outcomes of cancer surgery by creating cymatic images of the cells.
The term “cymatics” refers to the science of visible sound, based on the principle that when sound encounters a membrane, such as the surface of water, it renders the sound visible.
In a paper published in Advances in Intelligent Systems and Computing, Associate Professor Sungchul Ji and Professor Beum Jun Park of Rutgers University, in collaboration with John Stuart Reid, have put forward a novel classification method of differentiating between cancerous and healthy cells, referred to as the Planck–Shannon classifier (PSC) or the Planck–Shannon plot (PSP).
Health Europa digital editor, Stephanie Price, spoke to Reid to find out more about this research application for the CymaScope instrument, which is harnessing the science of cymatics to assist cancer surgeons in their work.
The CymaScope
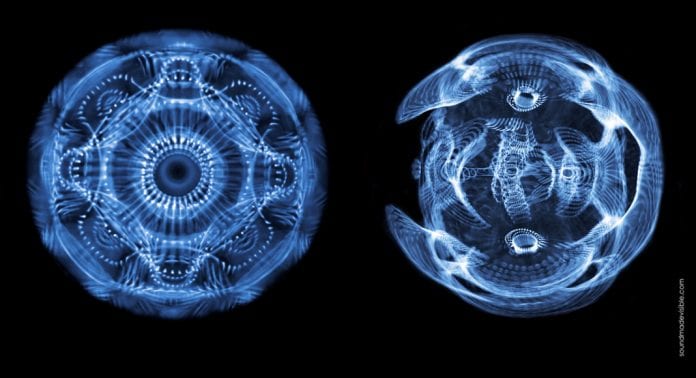
The CymaScope instrument makes sound visible – much like a fingerprint on glass – by imprinting the vibrations of sound onto the surface of pure water, which is then ‘dusted’ with light to make the resulting cymatic pattern visible. Such patterns are also known as “Faraday Waves.”
“The CymaScope transforms the sonic periodicities into water wavelet periodicities, literally making the sound visible,” says Reid.
“Pure, medical-grade water is injected into a small, fused-quartz cuvette. In the early days of development, we tried many different materials for the cuvette – but fused-quartz was discovered to provide the optimal results because at the microscopic level, the surface of fused-quartz has very few imperfections. From a scientific point of view this is very important to ensure that we accurately represent any inputted sound, creating an analogue or ‘model’ of the sound.
“When sound is injected into water it first appears in the epicentre of the cuvette, moves to the circular boundary, then reflects back. If those reflections incur imperfections, then the accuracy of the model would be compromised – which is why we use only quartz.”
Another important aspect of the CymaScope is that the cuvette and other mechanical parts of the instrument have a natural resonance that must be neutralised, or they would ‘colour’ the results.
“We are not interested in these natural resonances, so we tune them out with signal processing equipment to obtain a ‘flat frequency response’ – an accurate model of the inputted sound made visible. The CymaScope instrument can be employed to investigate many different sciences, including a wide range of medical sciences, such as haematology, cardiology, and neurology,” said Reid.
Applying the CymaScope in cancer surgery
All cells, with the exception of brain cells, have a natural respiration and this cell movement creates sounds inaudible to the human ear. The new science of sonocytology was discovered by Dr James Gimzewski in 2002. In 2017 Reid explored this concept further in collaboration with Professor Sungchul Ji, of Rutgers University, to differentiate the sounds of cancer cells from the sounds of healthy cells as a step toward other cancer-related research.
“Gimzewski discovered that every cell generates its own unique kind of “song.” Professor Sungchul Ji and I used this principle to listen in to the sound of healthy cells and compare them with the sounds of cancerous cells when their “song” was made visible with the CymaScope instrument,” said Reid.
“In general, cancer cells generate chaotic sounds, while healthy cells generate harmonious sounds. When we inject these sounds into the CymaScope instrument, the two types of cymatic patterns that appear are significantly different. With the healthy, harmonious sounds we see very beautiful, symmetrical patterns, and with the cancerous cells we typically see ugly, skewed patterns.
“The CymaScope uses a light ring to dust the water’s surface, and we utilise a conventional digital camera to capture the imagery. The set up for surgery would be significantly different, however, the basic concept would provide a camera feed direct to the surgeon’s spectacles.”
The images captured by the digital camera are quantitatively analysed using a generalised form of the Planck radiation formula, termed Planckian Distribution Equation (PDE). The new Planck-Shannon classification method, which is formulated based on PDE, has successfully distinguished between the cymatic/Faraday Wave images from the sounds of cancerous and healthy cells.
“As a result of this new technology we envisage a device that would be fitted to the eyewear of a surgeon. As the surgeon observes the tumour, they will use a Raman spectroscopy laser probe that would be scanned slowly across the tissues. During this process, the laser beam will be modulated by the sounds, not of one cell, but typically by thousands of cells, sending signals back to the laser sensor, which are then demodulated and injected into the CymaScope.
“In the eyewear of the surgeon, a cymatic picture would be seen as the laser beam is scanned from cancerous tissues to the healthy tissues – therefore, can very easily decide where to use their scalpel.”
Reid and Professor Ji aim to develop the method for more successful cancer surgeries and by automating histopathology.







